Book An Appointment
Physician Assistants
Physical & Occupational Therapists
KneeMRI ScansNon-OperativePhysiatry
Physical Therapy
Podiatry
Spine
Sports Medicine
TraumaUrgent Care
X-Ray Imaging

You don’t have to be a marathon runner to feel that nagging ache on the outside of your knee. The important thing? It might not actually be your knee. It might be a tight IT band, and unlike joint injuries, it requires a different kind of treatment focused on mobility and muscle balance.
Maybe it starts during your daily walk, or when you’re going up stairs. Perhaps it flares up when you get up from your desk or out of the car. It might even wake you up at night, pulsing in your outer thigh or hip, making it impossible to get comfortable. It doesn’t feel like an injury yet, the pain keeps coming back.
If this sounds familiar, there’s a good chance your iliotibial band (IT band) is involved. And the condition you might be dealing with is called IT Band Syndrome, a common cause of outer knee and hip pain that affects far more than just athletes.
Let’s walk through what’s happening in your body, why it hurts, and most importantly, what you can do to start feeling better.
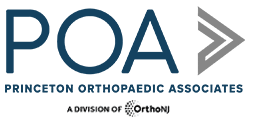
The iliotibial (IT) band is a thick, fibrous band of connective tissue that runs down the outside of your leg, from your hip to just below your knee. Think of it as a support strap that helps stabilize your knee and assist with hip movement.
When the IT band gets too tight, often due to repetitive movement, muscle imbalances, or poor posture, it can rub against the bone at the outer knee. This creates irritation, inflammation, and pain, commonly known as IT Band Syndrome (ITBS).
And while it’s often associated with athletes, it’s just as common in walkers, desk workers, parents, nurses, retail workers, and anyone who’s on their feet a lot, or not enough.
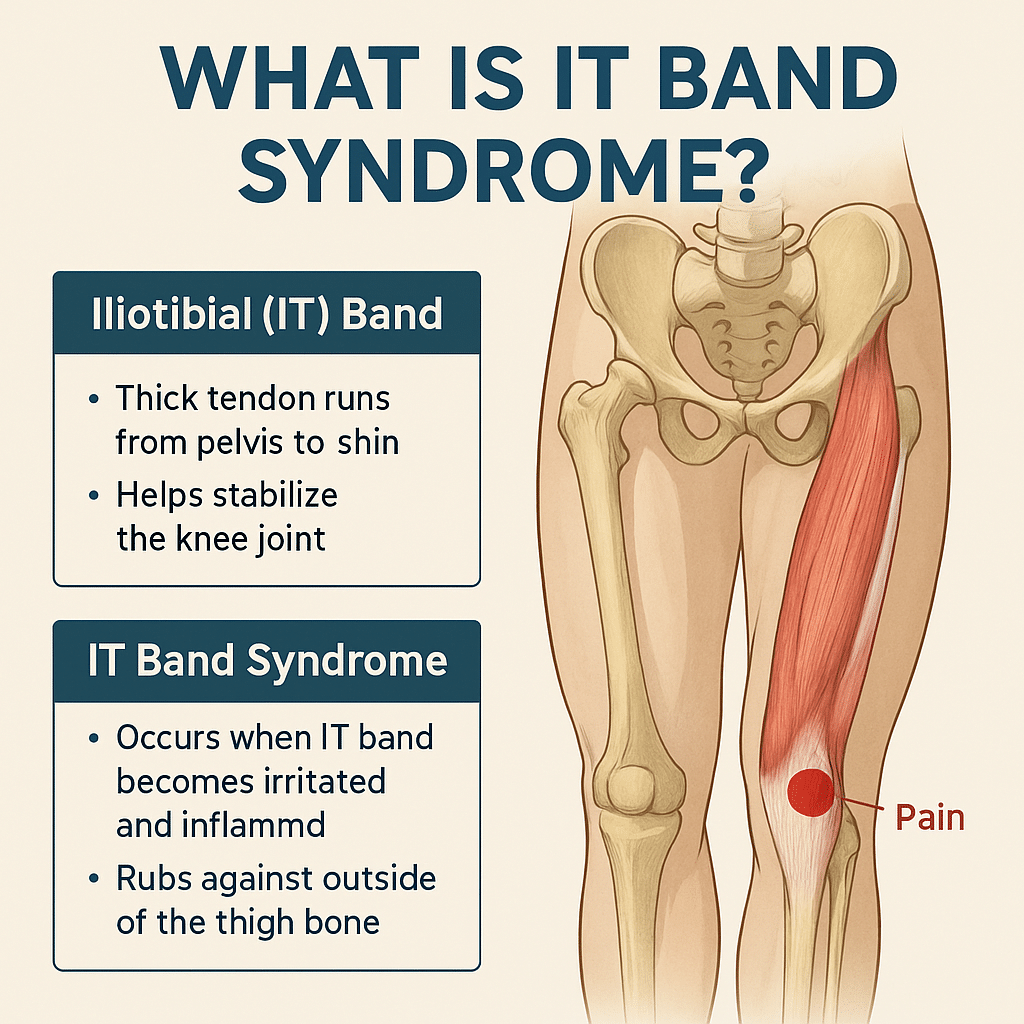
Here are common, real-world symptoms of IT Band Syndrome in everyday life:
These symptoms often start mild, but become more consistent if left unaddressed.
Even without intense training, everyday habits can contribute to ITBS:
While the core problem is the same (tightness and friction along the IT band), athletes often develop ITBS due to training volume and biomechanics. Common athletic triggers include:
IT Band Syndrome is common among:
💡 Tip for athletes:
Strengthen your hips and glutes, cross-train, and make sure your recovery matches your training load
.
The IT band isn’t a muscle, it’s actually connective tissue. That means:
Over time, the friction and inflammation can become chronic and much harder to treat.
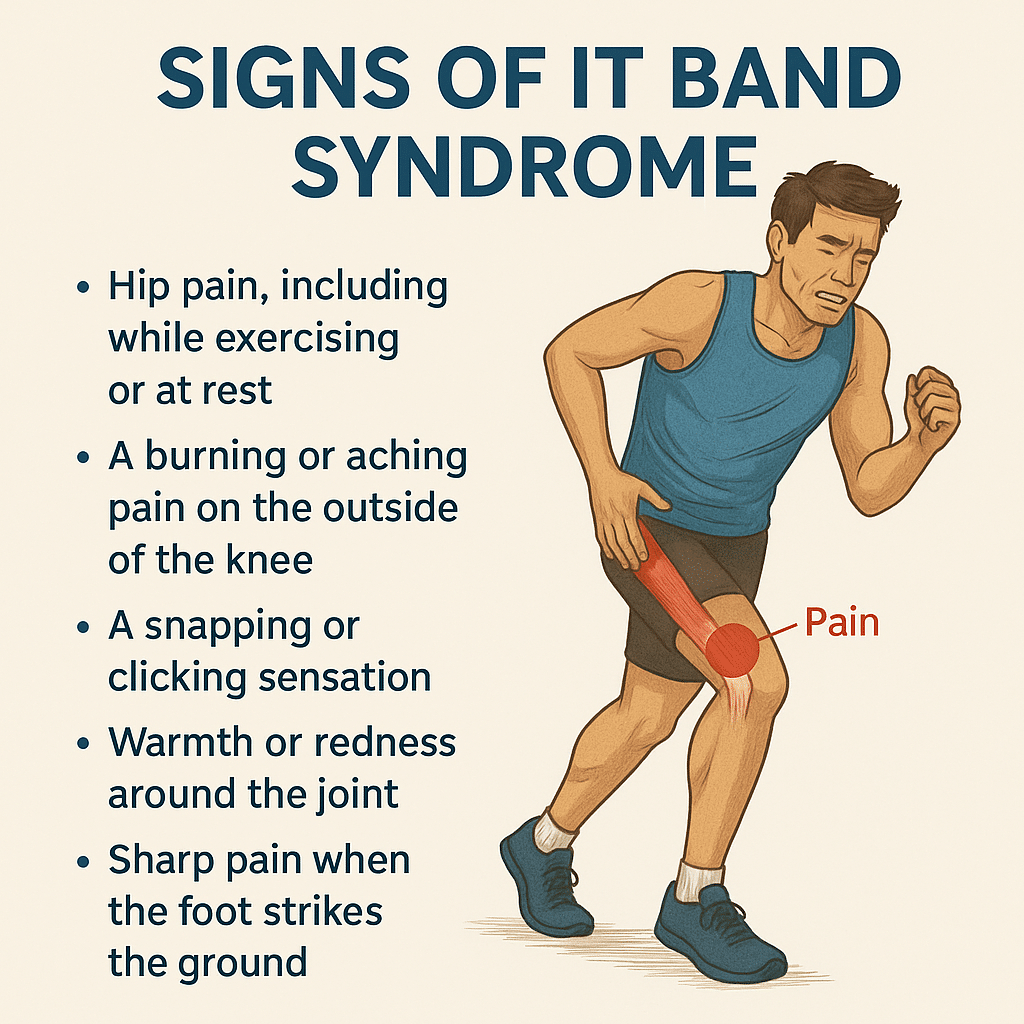
Treatment focuses on reducing inflammation, improving mobility, and correcting muscle imbalances.
✅ Pain Relief & Inflammation Control
The length of time to recover from IT Band Syndrome depends on how long you've had symptoms and whether you're treating the root cause:
2-3 Weeks
Rest and stretching may help quickly if caught early
4-6 Weeks
Requires active rehab including movement correction
2+ Months
Long-standing tightness or inflammation takes time to unwind
IT Band Syndrome doesn't just show up during workouts; it can quietly interfere with our daily routine, mobility, and overall comfort. Without treatment, ITBS can impact your:
And for athletes, it can put your training on pause or create a cycle of recurring injuries.
If you have been experiencing symptoms of IT Band Syndrome and you haven't found relief, you should consult with a specialist. Especially if:
At Princeton Orthopaedic Associates, we have physicians from multiple specialties that can help you get to the root of your tight IT band and help set you off on the path to recovery.
-Trained to treat soft tissue overuse injuries like ITBS
- Can differentiate between joint issues and soft tissue problems
- Often the best first stop for a non-surgical, comprehensive evaluation
- Focuses on functional movement and musculoskeletal pain
- Great at managing chronic pain or postural imbalances
-Ideal for cases involving compensations, gait issues, or mobility problems
- Best if ITBS has persisted or if you need advanced imaging or diagnostics
- Also helpful if you suspect other structural issues like meniscus, arthritis, or leg length discrepancy
- A physical therapist is often the next step after diagnosis for hands-on treatment and long-term recovery.
Our specialists will identify the root cause of your tightness, guide you through targeted corrective exercises, and help you improve how you move—not just mask the symptoms.
Whether you're training for a race or just trying to get through the workday without pain, IT Band Syndrome can be disruptive, but it's absolutely treatable. The key isn’t just stretching or resting, it's understanding why the IT band is tight and retraining your body to move in a healthier, more balanced way.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Whether you're experiencing discomfort in your hips due to inflammation or swelling, understanding this condition is vital to finding relief. Understanding the symptoms, causes, and treatment options for hip bursitis empowers you to take control of your health and well-being.

Hip bursitis, a form of arthritis, occurs when the bursa, fluid-filled sacs that cushion your joints, become inflamed and angry. Repetitive activities or injuries often cause it because this can result in pain and swelling around the hips, making everyday activities challenging. The result? Pain, tenderness, and swelling around your hip area. The first sign? Sharp pain at first that can settle into a nagging ache over time. Watch for swelling, warmth, and even redness around your hip.

Hip bursitis can develop from various factors:
Understanding the underlying causes can aid in prevention and management strategies. Think of hip bursitis as your body's way of saying "ouch" to alert you to overuse, injury, or poor posture. Even getting older can make you more prone to hip bursitis. Understanding the triggers can help you prevent future episodes. It's like your body's saying, "Hey, take it easy!"
Recognizing the symptoms of hip bursitis is essential for early intervention. Hip bursitis isn't shy about letting you know it's there.
If you are feeling pain, tenderness, or swelling around your hip, especially when you move, it might be hip bursitis.

Other signs include:
From pain and tenderness to swelling and altered gait, understanding these signs can help you seek timely treatment.
Hip bursitis isn't shy about making itself known. Activities like lying down for too long or walking distances can further irritate the bursa, adding "fuel to the fire." Some exercises and certain conditions, like rheumatoid arthritis or poor posture, can exacerbate hip bursitis, so keeping these in check is essential.
Managing hip bursitis involves a multifaceted approach to reducing inflammation and promoting healing. So, what can you do about it?
Fortunately, there are a few things you can implement yourself to find relief:
Resting the affected hip is crucial for reducing inflammation and promoting healing. Avoid activities that exacerbate pain and discomfort.
Heat therapy, such as warm compresses or heating pads, can help relax muscles. It can increase blood flow to the affected area, promoting healing and soothing pain.
Applying ice packs to the painful area can help reduce swelling and alleviate pain. Ice therapy can be done several times a day for about 15-20 minutes.
Over-the-counter pain relievers such as ibuprofen (Advil, Motrin) or naproxen (Aleve) can help alleviate pain and reduce inflammation.
Eating healthily and staying active can also help manage hip bursitis. Resting gives your hip a chance to recover, while a balanced diet supports overall healing. Stay active, but don't overdo it! If the pain persists, consult with an orthopaedic specialist for a tailored treatment plan.
There are other treatments your doctor may recommend for relief, such as:
Addressing hip bursitis with physical therapy gives you the advantage of tailored exercises that can work wonders, strengthening your hip and easing discomfort. Seeing a trained physical therapist is essential because knowing which exercises to avoid is just as crucial as knowing which ones to embrace.
Prevention is the key when it comes to hip bursitis.
Simple lifestyle changes, such as maintaining a healthy diet, regular exercise, and correcting posture, can help prevent the recurrence of this painful condition.
They say prevention is the best medicine, and it's true for hip bursitis too.
Early intervention is key to healing hip bursitis. Ice packs and rest can kickstart the process, followed by a visit to an orthopedic specialist for tailored guidance. If you feel like you're experiencing hip bursitis without relief, reach out and make an appointment with one of our orthopaedic specialists.

Please contact us! We'd love to help.
If you have hip pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
If you are experiencing hip bursitis, there are some specific things to avoid. Avoid things like running, deep squats, and leg lifts. Even cardio machines can be a no-go because they put too much pressure on your already irritated hips. Instead, focus on gentle stretches and movements that support rather than strain your hip joints.
Dealing with hip bursitis can be challenging, but it's not something you have to put up with forever; relief is within your reach with the proper knowledge and proactive steps. By understanding hip bursitis and its causes, recognizing its symptoms, and knowing how to address it effectively, you can manage it and get back to feeling like yourself again. Don't let hip bursitis hold you back.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.



Avascular necrosis, also known as osteonecrosis, occurs when your blood supply to a bone is disrupted due to various factors, leading to the death of bone tissue. This lack of blood flow deprives the bone of essential oxygen and nutrients, causing the bone to weaken and eventually collapse.
The symptoms of avascular necrosis can vary. It depends on the affected bone, but common signs include:
A sudden injury or trauma, such as a fracture or dislocation, can damage blood vessels and interrupt blood flow to the bone.
Certain chronic conditions, such as sickle cell anemia, lupus, and diabetes, can affect blood vessels and increase the risk of avascular necrosis.
Long-term use of high-dose corticosteroids, often used to treat conditions like arthritis or asthma, can disrupt blood flow to the bones.
Heavy alcohol use can impair blood circulation and weaken bones, increasing the risk of avascular necrosis.
Some medical treatments, like radiation therapy, can damage nearby blood vessels, leading to avascular necrosis. Additionally, excessive pressure on certain joints, such as the hips or knees, can restrict blood flow and contribute to the condition.
Avascular necrosis (AVN) can affect various body parts, particularly those highly reliant on strong, healthy bones and good blood circulation.
AVN frequently occurs in the hip joints, particularly in the femoral head (the ball part of the hip joint). Hip AVN can lead to significant pain, stiffness, and reduced mobility.
While less common than hip AVN, the knee joint can also be affected. AVN in the knee can cause pain, swelling, and difficulty with movement.
AVN can affect the shoulder joint, particularly the humeral head (the ball part of the shoulder joint). Shoulder AVN may cause pain, limited range of motion, and weakness.
AVN can occur in the talus bone within the ankle joint. Ankle AVN can cause pain, swelling, and difficulty walking.
Although less common, AVN can also affect the jawbone (mandible or maxilla). Jaw AVN can lead to jaw pain, difficulty chewing, and other oral health problems.
AVN can affect the vertebrae in the spine, particularly in the lumbar spine, which is the lower back region. Spinal AVN can cause back pain, stiffness, and, in severe cases, neurological symptoms due to compression of the spinal cord or nerves.
These areas are particularly vulnerable to AVN because they contain weight-bearing joints or are subjected to significant mechanical stress. Additionally, the blood supply to these areas may be compromised due to their anatomical location or underlying conditions, making them more susceptible to AVN. However, AVN can occur in any bone in the body, depending on the underlying causes and risk factors.

Diagnosis typically involves a combination of your medical history, a physical examination, and imaging tests such as X-rays, MRI, or CT scans. Treatment options depend on the stage of the condition. They may include medications to relieve pain, physical therapy to improve joint function, and surgical procedures such as core decompression, bone grafting, or joint replacement.
Early detection and intervention are crucial to managing avascular necrosis and preventing further complications. If you're experiencing symptoms or have concerns about AVN, consult a healthcare professional for evaluation and appropriate treatment.
Early detection and intervention are crucial in managing avascular necrosis and preventing further complications. If you suspect you have AVN or experience symptoms, promptly seeking medical attention is crucial. It's important to consult with a healthcare professional promptly for appropriate diagnosis and treatment, and at Princeton Orthopaedic Associates, our specialists can provide a comprehensive evaluation, listen to your concerns, and build a custom treatment plan, personalizing it to your needs.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
Specializing in bone disorders, orthopedic surgeons offer treatments ranging from medications to surgical procedures like core decompression or joint replacement.
Physiatrists focus on nonsurgical treatments like physical therapy to improve joint function and manage pain.
Are you worried about AVN affecting your hip or another joint? It's crucial to consult with a specialist, such as an orthopedic surgeon, to develop a personalized treatment plan. Early detection and proper management can significantly improve outcomes and quality of life for individuals with AVN.
Although it's less common compared to other causes like trauma or medication use, some genetic factors may predispose individuals to AVN, making them more susceptible to the condition.
Research suggests that specific genetic mutations or variations may increase the risk of AVN. For example, mutations affecting proteins that maintain blood vessel function or regulate bone metabolism could potentially contribute to AVN development. Additionally, some hereditary conditions, such as sickle cell disease, can increase the likelihood of AVN.
While genetics may play a role, a combination of genetic predisposition and environmental factors, such as trauma, medication use, or other medical conditions, influence the development of AVN. The exact genetic factors contributing to AVN are still being studied, and more research is needed to understand them fully.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Do you experience pain and tenderness in your side hip? You may be suffering from trochanteric bursitis, a condition that causes inflammation of the hip bursa. This explains why it’s sometimes referred to as "hip bursitis." Having knowledge about the symptoms, treatment options, and preventive measures is essential for reducing discomfort in those who suffer from this common condition. In this post we'll examine exactly what Trochanteric Bursitis is all about – its causes, possible treatments and methods of prevention. By understanding both the medical aspects of the issue as well as practical solutions to managing it in daily life you can find great relief - helping promote healthier hips activities going forward!

Trochanteric Bursitis is a condition in which the bursa, a small fluid-filled sac, located on the outer side of our hip joint becomes inflamed. This can cause severe pain and discomfort. Although the condition is commonly associated with athletes and runners, it can develop in anyone who puts prolonged pressure on their hips. People who have recently started a new exercise routine, have poor posture, or stand for extended periods of time are at risk of developing Trochanteric Bursitis. It can also affect women more commonly than men due to the structure of their pelvis. Therefore, it is important to maintain good posture and consult a doctor if you suspect you have Trochanteric Bursitis to prevent the condition from worsening.

Trochanteric bursitis is a condition that causes pain and discomfort in the hip area. It occurs when the bursae, small fluid-filled sacs that act as cushions between bones and tendons, become inflamed. This inflammation can be caused by overuse, injury, or underlying conditions such as arthritis. Symptoms of trochanteric bursitis can include pain in the hip or buttock area that worsens with activity, tenderness to the touch, and difficulty sleeping on the affected side. In some cases, the pain may radiate down the leg. While trochanteric bursitis can be a frustrating and painful condition, there are treatments available to help manage the symptoms and improve quality of life.

Trochanteric bursitis can cause a lot of discomfort and pain in the hips. Knowing how to diagnose it can make a huge difference in finding relief from this condition. One of the most reliable ways to diagnose trochanteric bursitis is through a physical examination by a medical professional. They will assess the level of inflammation on the outermost facet of the hip and the level of joint pain. It is also helpful to discuss how long the pain has been present, any previous injuries, and the type of activities that may have led to the pain. Diagnostic imaging like X-rays or MRIs may be necessary to visualize the soft tissue and determine if there is any structural damage. An accurate diagnosis is the first step towards getting the right treatment and alleviating the pain caused by trochanteric bursitis.
Trochanteric bursitis, commonly known as hip bursitis, is a painful condition that occurs when the small sacs of fluid that cushion the hip joint become inflamed. It can make it difficult to perform everyday activities and significantly reduce quality of life. Fortunately, there are several treatments available to help manage the symptoms of trochanteric bursitis. These include physical therapy, anti-inflammatory medications, corticosteroid injections, and in some cases, surgery. Physical therapy can help strengthen the muscles around the hip and improve flexibility, while anti-inflammatory medications can reduce swelling and pain. Corticosteroid injections can provide more immediate and long-lasting relief, but surgery may be necessary if other treatments do not provide adequate relief. With the right care plan in place, those dealing with trochanteric bursitis can manage their symptoms and get back to their regular routines.
Trochanteric bursitis is a common condition that can cause a lot of discomfort and inflammation, but luckily, there are several home remedies you can try to help relieve the pain and discomfort. One remedy is applying heat or ice to the affected area, depending on what feels best for you. Another is gentle stretching exercises to help loosen up the muscles around the hip. In addition, try to avoid activities that aggravate the condition, such as excessive running or sitting for long periods of time. Essential oils, such as ginger and peppermint, may also help ease the pain and inflammation. With these natural remedies on hand, you can find relief from trochanteric bursitis and get back to your daily routine in no time.
The hip joint is a vital part of movement, but it can also be a source of pain and discomfort. Trochanteric bursitis, a common condition caused by inflammation of the bursa over the hip bone, can restrict mobility and hinder the ability to carry out everyday activities. Fortunately, there are exercises that can help strengthen the muscles around the hip and reduce the risk of recurring bursitis. These exercises include stretches to help increase flexibility, as well as resistance exercises that target the glutes and hips. With dedication and consistent practice, these exercises can help alleviate pain and enable greater mobility, ultimately leading to a healthier, more active lifestyle.
In conclusion, Trochanteric Bursitis is a painful condition that can affect the hips of people of all ages, sizes and genders. It affects those who are active and non-active alike. The disorder may be quite painful but it can be treated effectively with rest and prescription medications to reduce inflammation. Home remedies like hot or cold compresses, stretching exercises, and massage therapy can also help manage pain associated with Trochanteric Bursitis. Exercise is key for strengthening the muscles around the hip joint and prevention of further recurrence of this malady. Having an understanding of what Trochanteric Bursitis is and its common cause, symptoms, treatment options, home remedies and how to prevent it from recurring will serve individuals well in dealing with this disorder. By knowing when to seek medical care for this condition you can avoid more serious complications down the road enabling you to live life happily without discomfort or disability caused by Trochanteric Bursitis
When it comes to the health of your hips, bursitis is not something you want to hear. But if you have ever experienced it, you know how much of a nuisance it can be. Bursitis is inflammation of one or more bursa—fluid-filled sacs located beneath your skin in certain spots, most notably around your hips. This condition can make even the simplest tasks extremely painful. Prolonged bursitis can even result in permanent damage. Fortunately, there are several things you can do to help prevent bursitis from developing or coming back. But if you suspect that you have developed bursitis and are ready to take action to get rid of it for good, this article will help get you started on the right track. Here, you’ll learn about the common causes and symptoms of hip bursitis as well as various treatment options that might be right for you.
Bursitis is a form of arthritis that causes inflammation of the bursa. Bursa are small sacs of fluid — like miniature joints — that help cushion the joints and reduce friction and pain. Bursitis can occur in the shoulder, knee, hip and even the elbow. If the bursa becomes irritated and swollen, it can become a bursitis. People who do repetitive motions such as people who lift weights or who sit at a computer all day are at risk for bursitis. If you have an inflamed bursa, you may experience pain and swelling around the area where the bursa is located. The most common areas in which bursitis develops are the shoulder, elbow, knee and hips. Bursitis can also develop in your feet, which is referred to as plantar bursitis.
Bursa are small pouches filled with fluid that sit between your muscles, tendons and bones. Some bursa help reduce friction between the bones and may be referred to as “dynamic” bursa, such as the ones found around the hips. While others are known as “static” bursa and are located near joints, helping to keep the bones from rubbing against each other. The buildup of pressure in this fluid-filled sac can cause inflammation, which is known as bursitis. Bursitis can be caused by a number of factors, including injury, overuse, infection or poor posture. You are most at risk for bursitis if you have a job that requires repetitive motions, such as manual labor or work on a computer, as well as those who participate in activities that require a lot of jumping or quick movements, such as sports or dancing.

The exact cause of bursitis is unknown, but it can develop when a sudden increase in pressure occurs within a bursa sac. This often happens when the bursa are overused or irritated.
Common causes of bursitis include:

Since bursitis is an inflammatory-based condition, treatment includes reducing inflammation by following a warm compress or ice pack routine while resting as much as possible. In addition, you may want to consider following a healthy diet and lifestyle to further help prevent the condition from recurring.
Hip bursitis can be a painful condition that can make even the simplest activities difficult. Luckily, there are several things you can do to help prevent it or reduce its severity, such as following a healthy diet, exercising regularly and changing your posture. If you think you may have developed bursitis, you should see your doctor for treatment.
Hip bursitis is a painful condition caused by inflammation of the small sacs that cushion the hip joint. It can be painful enough to limit mobility, including walking upstairs or getting out of a deep chair. The good news is, there are several treatment options available for hip bursitis. The experts at Princeton Orthopaedic Associates can find the right treatment plan for your pain.
Hip bursitis, also known as trochanteric bursitis, is an inflammation of the bursa, tiny fluid-filled sacs near the hip joint called the greater trochanter. This joint is the area where the head of the femur (thigh bone) meets the long part of the bone. This area has a bursa that cushions the femur and its joint with the pelvis (hip bone).
There are several possible causes of hip bursitis:
Symptoms can include pain or stiffness, particularly when climbing stairs or standing from a deep chair or cushion. The pain tends to be on the side of the hip but can radiate around to the outside of the buttock or the hip.
Treatment of hip bursitis can vary depending on the severity of the pain and inflammation. That’s why it’s essential to assess your pain level before deciding on the best course of treatment. That treatment can range from over-the-counter pain medications to surgery.
Treatment begins with nonsteroid anti-inflammatory drugs (NSAIDs) such as ibuprofen. It also may require rest of the joint, which means not standing for long periods or not climbing stairs.
The next step is corticosteroid injections, which quickly reduce inflammation and pain. Relief can last several weeks to a few months.
Physical therapy can build up strength in the joint, straighten the joint, improve posture, and reduce pain and inflammation. We can also use physical therapy sessions to recover from bursitis and help prevent it from recurring.
If these methods fail to alleviate or eliminate the pain, surgery may be necessary. During surgery, the surgeon removes the bursa causing the problem. The surgery can be performed arthroscopically using only small incisions, which means faster healing for the patient.
Surgery for hip bursitis is rare and is only done in extreme cases. In most cases, other treatment methods bring sufficient relief.
© 2025 Princeton Orthopaedic Associates. The contents of PrincetonOrthopaedic.com are licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. Copying without permission is strictly forbidden. Privacy Policy | Accessibility