Book An Appointment
Physician Assistants
Physical & Occupational Therapists
KneeMRI ScansNon-OperativePhysiatry
Physical Therapy
Podiatry
Spine
Sports Medicine
TraumaUrgent Care
X-Ray Imaging

Lower back pain is common, and the right movements can make a big difference. This guide walks you through simple mobility drills, gentle stretches, and core-strengthening exercises, plus how often to do them, how to stay safe, and when to see a specialist at Princeton Orthopaedic Associates.

These movements should feel gentle and controlled. You may notice a comfortable stretch or mild muscular effort, but you should not experience sharp, stabbing, or worsening pain at any point during the exercise. If you feel uncomfortable, ease back, rest briefly, and check your form. Move slowly, keep your movements smooth, and breathe steadily throughout each position.

Begin with slow, comfortable movements to ease the back and improve blood flow throughout the spine. Move with control, staying in a pain-free range, and stop if anything sharp or increasingly uncomfortable appears. For most moves, aim for about five to ten deliberate repetitions unless otherwise noted.
Strong hips and a steady core help unload irritated tissues in the lower back and support your spine during daily tasks. Perform each movement with deliberate control, paying attention to alignment and how your body feels. If any symptom worsens, stop the exercise and reassess your form. Aim for two to three sets, with 30 to 60 seconds of rest between sets.
Tight hips or hamstrings can pull on the pelvis and increase back strain. Hold each stretch 15 to 30 seconds, repeat 2 to 3 times, and keep breathing.
Use this plan as a flexible starting point and adjust it based on how you feel and what you can tolerate. Prioritizing consistency and gradual progress matters more than pushing for fast gains. Listen to your body, and modify days, reps, or rest as needed to stay comfortable and avoid flare-ups.
| Day | Mobility | Strength | Stretch | Notes |
|---|---|---|---|---|
| Mon | Pelvic tilts, trunk rotations | Bridge, clamshell | Hamstrings | Easy start, 1 to 2 sets |
| Tue | Cat to cow | Bird dog | Hip flexors | Focus on form |
| Wed | Child’s pose | Dead bug | Piriformis | Optional walk 10 to 20 min |
| Thu | Pelvic tilts, trunk rotations | Bridge, clamshell | Hamstrings | Add 1 to 2 reps if comfortable |
| Fri | Cat to cow | Bird dog | Hip flexors | Short and easy |
| Sat | Choice mobility | Plank holds | Piriformis | Walk or light activity |
| Sun | Recovery | — | Gentle stretch | Listen to your body |
Most back pain improves with gentle activity and careful pacing, but some warning signs require medical input sooner rather than later. If your symptoms persist beyond a short period, intensify, or there are new concerns, seek medical guidance promptly. The list below describes red flags that warrant evaluation by a clinician.
If your symptoms aren’t improving, our team can evaluate your movement, identify the source of pain, and build a program that fits your goals. Most people do well with focused physical therapy, activity modification, and a progressive home plan.
If you’re unsure where to start, schedule an exam with our spine or physical therapy team. We’ll help you understand what’s safe, how to progress, and when additional options are appropriate.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Elbow tendinopathy is a common overuse injury that causes pain and tenderness in the tendons around the elbow. It happens when these tendons—connecting muscle to bone—become irritated from repeated stress. In this blog, you’ll find simple home treatments that can help relieve symptoms and learn when it’s time to see a specialist.
We’ll cover what causes elbow tendinopathy, the differences between lateral and medial types, practical home care tips, rehab strategies like strengthening and stretching, and when injections or surgery might be needed.

Elbow tendinopathy is an overuse condition where the tendons around your elbow become irritated. Tendons connect muscles to bone, and when they’re overloaded they can be painful and tender.
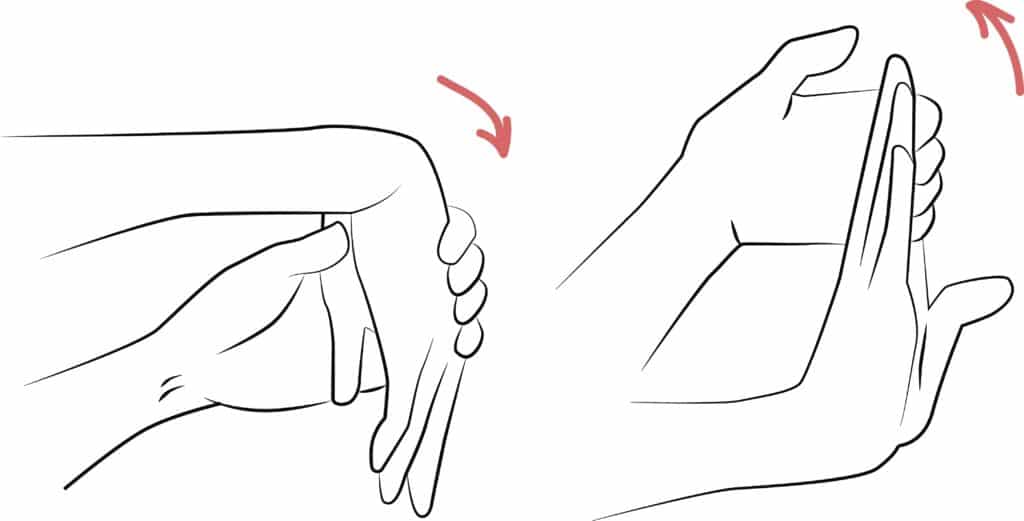
There are two common forms. Lateral elbow tendinopathy affects the outer elbow and is often called tennis elbow. Medial elbow tendinopathy affects the inner elbow and is often called golfer's elbow. Both share similar causes and treatments.
Repeated or forceful wrist and arm motions are the usual culprits. These motions create small tears and inflammation in the tendon where it attaches to the bone.
Many people feel better with early conservative care. Try these measures for several weeks while monitoring symptoms.
Physical therapy is the mainstay for lasting relief. A therapist will show you targeted exercises to rebuild tendon health and correct movement patterns.
If symptoms persist despite conservative care, your provider may discuss additional options. These are considered after a careful evaluation.
Recovery varies with how long symptoms have been present and how consistently you follow rehab recommendations.
| Stage | Typical Timeframe | What to Expect |
|---|---|---|
| Acute | 1 to 3 weeks | Rest, ice, activity modification bring notable relief |
| Rehab | 4 to 8 weeks | Therapy and strengthening restore function for most people |
| Chronic | 2 months or longer | May need advanced treatments and extended rehab for full recovery |
Once your pain improves, keep working on strength, flexibility, and technique. Those steps reduce the chance that tendinopathy will come back.
Contact our team if pain lasts despite home care, limits your daily tasks, or if you’re losing strength. We’ll evaluate your elbow, identify the root cause, and recommend a personalized plan.
Schedule an exam with one of our sports medicine doctors or physical therapists to get targeted treatment and a clear recovery plan.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Good posture means your head, shoulders, and hips line up with your spine. This helps your body work well and move with less pain. Small, steady changes can add up over days and weeks. This guide explains why posture matters, common reasons it slips, safe exercises, and quick ergonomic setup ideas you can use at home or work to feel better and move more easily.

Good posture helps distribute forces evenly across your joints and muscles. When posture is poor, some muscles take on extra work while other areas weaken, which can lead to neck, shoulder, or back pain. The encouraging part is that steady, small changes usually lead to meaningful improvements.

Good posture means your head, shoulders, and hips line up so your spine is supported and muscles can work efficiently. It doesn’t mean you must sit perfectly rigid. Instead, aim for balance: a neutral spine with relaxed shoulders and an engaged core.
When your posture is balanced, less stress sits on joints and soft tissues, and you’re less likely to develop pain from overuse or compensatory movement patterns.
Posture affects pain, breathing, and how you move. Slouching can make neck and upper back muscles work harder. It can also change how your shoulders and hips move, which may lead to recent or gradual pain.
These choices are low-risk and can be done at home. Start gently and increase repetitions over weeks as you feel stronger. Evidence from major guidelines supports regular practice, with adults typically performing strengthening 2 to 3 days per week and stretches held for 20 to 30 seconds, gradually increasing as tolerated. (ACSM guidelines 2023)

People improve at different speeds. Small changes can show up in a few weeks if you practice regularly. Bigger, longer standing posture problems take longer to improve and may need a tailored plan. A steady mix of simple strengthening moves, daily posture habits, and help from a clinician or physical therapist can help you move better and reduce pain.
| Issue | Typical time to notice change | Notes |
|---|---|---|
| Minor slouching | 2 6 weeks | Daily breaks and basic exercises usually help. |
| Moderate postural imbalance | 4 6 weeks | Requires consistent strengthening and ergonomic changes. |
| Long-standing posture-related pain | 2+ months | Often needs a tailored program from a clinician or physical therapist. |
Try the self-care tips for a week or two. See a specialist sooner if pain limits your daily activities, if you change how you walk or move to avoid pain, or if home measures don’t help.
| Provider | What they help with |
|---|---|
| Primary care or sports medicine | Initial evaluation and recommendations for non-surgical care |
| Physical therapist | Hands-on treatment, personalized exercise programs, posture training |
| Physiatrist | Complex movement problems, chronic pain management, coordinate care |
At Princeton Orthopaedic Associates, we assess the root cause of posture problems and work with you to build a practical plan. We focus on restoring function and helping you return to activities with less pain.
If you need help customizing a program or you have persistent pain, schedule an exam so we can evaluate you and design a specific plan.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Gout is a common type of inflammatory arthritis that causes sudden, intense joint pain and swelling. In this guide, you will learn what gout is, why it happens, who is at higher risk, how we diagnose it, and the treatments that help you feel better and prevent future flares.

Gout happens when uric acid builds up in the blood and forms needle-like crystals inside a joint. Your immune system reacts to those crystals, which triggers sudden pain, redness, heat, and swelling. The big toe is the classic spot, but gout can affect the midfoot, ankle, knee, wrist, fingers, and elbow.
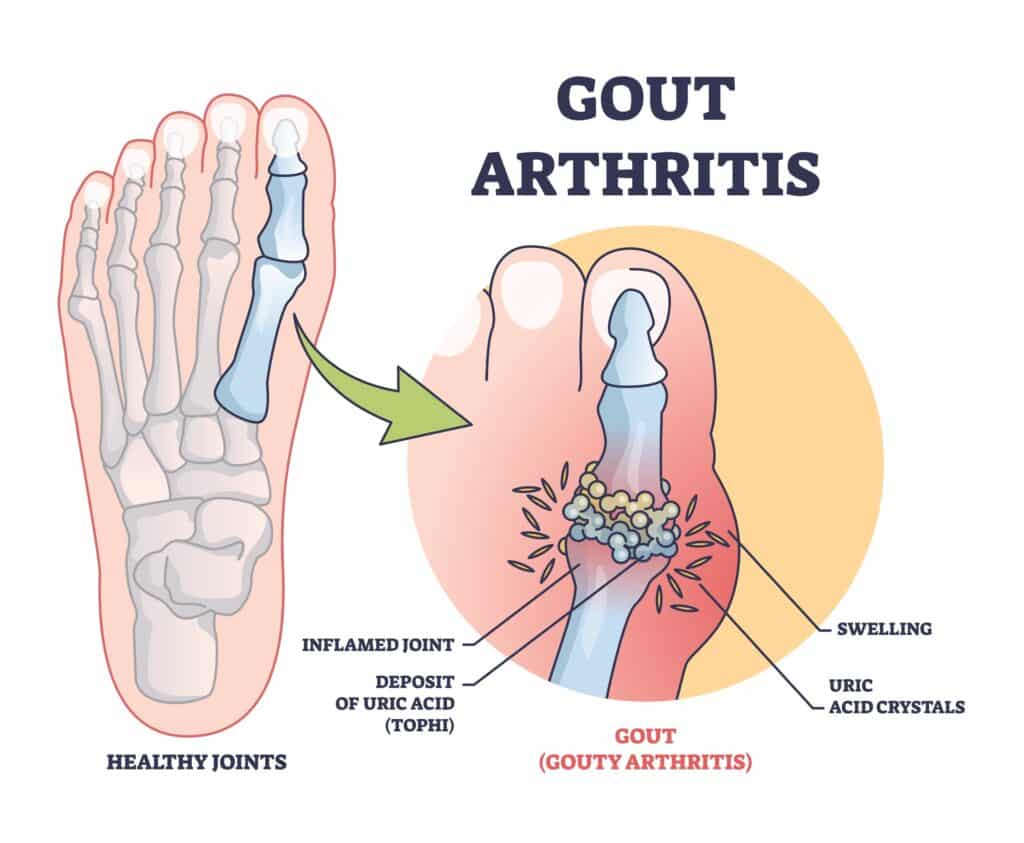
Uric acid forms when your body breaks down purines, which are found naturally in your tissues and in certain foods. When production is high or your kidneys don’t clear enough uric acid, crystals can deposit in joints and surrounding tissues. Cold areas like the big toe are common sites for crystal formation.
If you notice a new hot, swollen joint or have repeated gout flares, seek care promptly from a clinician or urgent care provider. Early evaluation helps confirm that gout is the cause, guides fast pain relief, prevents infection or other problems, and protects the joint from lasting damage. A clinician will review your health history and medicines to choose safe, effective treatment and avoid drug interactions.
During your visit, a clinician will look at the painful joint and review your overall health, symptoms, and medicines. The best way to confirm gout is to take a tiny sample of joint fluid and check it under a microscope for uric acid crystals. This test helps rule out infection and other problems that can look like gout.
Flares respond best when treatment starts early. The main goal is to ease pain quickly, reduce swelling, and lower inflammation while protecting the affected joint from more harm. Your doctor will tailor medicines to your health history and current medicines to ensure safety and effectiveness and help you return to daily activities.
Do not stop your long-term urate-lowering medicine during a flare unless your doctor advises it. Let us know at the first sign of a flare so we can tailor treatment to your health history and medications.
If you have repeated flares, tophi, kidney stones from uric acid, or moderate to advanced chronic kidney disease, you may benefit from urate-lowering therapy. The aim is to keep your blood uric acid below target so crystals dissolve and flares fade over time.
| Topic | Key Points |
|---|---|
| Who Should Start Urate-Lowering Therapy | 2 or more flares per year, tophi, uric acid kidney stones, or chronic kidney disease stage 3 or higher |
| First-Line Medicine | Allopurinol is typically first choice. Start low and increase gradually. Febuxostat is another option if needed. In patients with established cardiovascular disease, febuxostat carries an FDA boxed warning for increased risk of cardiovascular death. Use only after shared decision-making, and consider allopurinol first. Allopurinol can rarely cause severe cutaneous adverse reactions. Consider HLA-B*58:01 testing in high-risk groups (e.g., Han Chinese, Thai, Korean patients with CKD, and African American patients) before starting therapy. |
| Other Options | Probenecid may help if kidney function is adequate. Pegloticase is reserved for severe, refractory cases. Less effective with moderate-to-severe CKD; avoid or use cautiously in patients with a history of uric acid kidney stones; review for drug–drug interactions. |
| Target Uric Acid | Under 6 mg/dL is the usual goal. Under 5 mg/dL may be used if tophi are present. |
| Flare Prevention When Starting Therapy | Low-dose colchicine or an NSAID is often used for several months to reduce flare risk during dose adjustments. |
Our team evaluates the painful joint, confirms the diagnosis, and builds a treatment plan that eases pain fast and prevents future attacks. When appropriate, we can perform joint aspiration or an image-guided injection and coordinate long-term urate-lowering therapy with your broader care team.
If you think you're having a gout flare or you've had recurrent attacks, schedule an evaluation. Getting ahead of flares now helps protect your joints for the long term.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Hand cramps are sudden, involuntary squeezes of the muscles in your hand or fingers. They can happen during activity or at rest and often respond to simple measures, but sometimes they point to an underlying issue that needs professional care.
A hand cramp is a tight, often painful contraction of one or more hand muscles that you cannot relax immediately. They usually happen without warning and can last from a few seconds to several minutes.

Several everyday factors can make hand cramps more likely. Often more than one factor is involved.
Hand cramps can vary from a mild tightness to a painful spasm. They may affect one finger, several fingers, or the whole hand. Symptoms often come on suddenly and can interfere with normal hand use until the muscle relaxes.
If a cramp starts, try these simple measures to help the muscle relax. These steps are safe for most people and often work quickly.
Note: If cramps happen frequently, or are severe, it is important to get a medical review to find the cause.
Preventing hand cramps often means addressing how you use your hands and caring for overall muscle and nerve health. Small daily changes can reduce episodes significantly.
See a clinician if cramps are persistent, frequent, worsening, occur at rest without clear triggers, or are accompanied by numbness and weakness. Those signs may indicate a nerve or systemic issue that needs evaluation.
| Specialist | When to Choose | Notes |
|---|---|---|
| Primary Care Provider | First evaluation, blood tests, medication review | Good starting point to rule out common causes |
| Orthopaedic Hand Specialist | Suspected structural or nerve problems in the hand or wrist | Can order imaging and advanced hand exams |
| Physical or Occupational Therapist | Rehabilitation, stretching, strengthening, ergonomics | Helps correct movement patterns and build hand endurance |
| Neurologist | Frequent cramps with weakness or other neurological signs | Assesses nerve disorders and coordination |
Treatment depends on the cause. Many people improve with conservative measures. In select cases, targeted therapies may be recommended.
These gentle stretches may reduce tightness and build resilience. Stop if they cause sharp pain and check with a clinician if you have an injury.
Recovery varies by cause and how soon you begin appropriate care. Many people improve within days when the issue is temporary. If cramps come from nerve compression or a chronic condition, recovery may take weeks to months with therapy and targeted treatment.
| Typical Pattern | Timeframe | What Helps |
|---|---|---|
| Acute, activity related | Days to weeks | Rest, hydration, stretching |
| Recurrent with overuse | Several weeks | Ergonomic changes, therapy |
| Nerve-related (peripheral nerve compression) or other nerve-related causes | Weeks to months | Specialist evaluation and targeted care |
Most people can manage occasional cramps with simple self-care and small changes to daily routines. If cramps limit your work or hobbies, we can help find the right plan so you can stay active and comfortable.
If your cramps are persistent or troubling, schedule an exam with one of our hand specialists. We will review your history, examine your hand, and recommend tests or therapy if needed. Together we will create a plan tailored to your needs.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.

Penn Orthopaedics and Princeton Orthopedic Associates have announced a new strategic alliance in an effort to enhance and continue to improve orthopaedic care to patients in New Jersey and Pennsylvania. As part of the Penn Medicine Orthopaedic Specialty Network, physicians and surgeons at each entity will work collaboratively across state lines to expand patients’ access to highly specialized orthopaedic care, while improving care team communication and processes and collecting data to help physicians advance clinical research and care.
As part of this alliance, Princeton Orthopedic Associates’ 25 physicians and five practice locations will further expand the footprint of the Penn Orthopaedics network of affiliated physicians and hospitals – which also includes Cape Regional Medical Center in New Jersey and Bayhealth in Delaware – to reach to those in central New Jersey.
“When looking for a partner in the tri-state area, we focused on finding an institution which shared our commitment to providing the highest quality care, to creating an environment where our patients and their families would feel most comfortable and cared for, and to aligning with a group that would be unwavering during the changing healthcare climate,” said Stuart Levine, MD, president of Princeton Orthopedic Associates. “In Penn Medicine Orthopaedics, we found the level of dedication and personalized patient care that we had been looking for in a regional partner.”
“One of the main goals of the Penn Orthopaedics team is to provide the best orthopaedic care, whether a joint replacement, a hand transplant or a cartilage repair, to the greatest number patients,” said L. Scott Levin, MD, FACS, chair of Orthopaedic Surgery and a professor of Plastic Surgery at Penn Medicine. “The partnership with Princeton Orthopedic Associates, the leading community group in central New Jersey, was a natural fit, as our missions are built on the same ideals: taking the best possible care of our patients and forging strong relationships with them and their families, and advancing practice through clinical innovation.”
Princeton Orthopedic Associates is already one of the largest orthopaedic practices in New Jersey, serving primarily those in Mercer County and by proximity to Pennsylvania, those in northern Bucks County.

We are pleased to announce the addition of William H. Rossy, M.D., and Brian M. Culp, M.D. to our practice. Dr. Rossy is a Sports Medicine specialist, and Dr. Culp specializes in Total Joint Replacement. Both physicians are Fellowship Trained Orthopaedic Surgeons and are currently accepting new patients.
Dr. William H. Rossy is a board-certified orthopedic surgeon with a sub-specialty interest in Sports Medicine and the treatment of orthopedic trauma. Dr. Rossy specializes in the management of all sports-related injuries. He has advanced training in arthroscopic and open management of injuries sustained to athletes at all levels--from high school up through professional. He worked as an assistant team physician for the New England Patriots, Boston Red Sox, and Boston Bruins during his fellowship.
Dr. Rossy has vast experience in treating ailments of the shoulder as well as complex, multi-ligamentous injuries of the knee. He also has a particular interest and specialized training in hip arthroscopy and cartilage restoration procedures. He aims to return patients to desired sport and/or activity predictably and reliably by offering the most advanced surgical techniques.
Dr. Culp is excited to return to New Jersey, where he completed his general surgical internship and his orthopedic surgery residency at UMDNJ Robert Wood Johnson University Hospital. He is returning following a one-year Fellowship at RUSH in Chicago doing a fellowship in adult reconstructive surgery.
Dr. Culp brings unique expertise on knee replacement surgery, including minimally invasive partial and total knees as well as complex revision surgery. He also performs minimally-invasive hip replacement surgery from anterior and posterior approaches as well as complex revisions. His practice focuses on patients of all ages who have advanced degenerative disease.
Dr. Culp offers outpatient joint replacement surgery to the appropriate candidates. Dr. Culp will be offering the outpatient total joint replacement surgery at both the UMCP Monroe Surgical Center and the UMCP Surgical Center on the hospital campus in Plainsboro.
Princeton Orthopaedic Associates is proud to announce we have been chosen by Blue Cross Blue Shield of New Jersey to be a Tier 1 provider in their OMNIA Health Plans. The Group was selected based on patient satisfaction, quality of clinical care and commitment to value-based healthcare. Patients enrolled with OMNIA Health plans will see lower co-payments and deductibles by utilizing a Tier 1 provider like Princeton Orthopaedics Associates. As always our commitment is to your excellent Orthopaedic care.
To learn more about the OMNIA Health plans please click below:
© 2025 Princeton Orthopaedic Associates. The contents of PrincetonOrthopaedic.com are licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. Copying without permission is strictly forbidden. Privacy Policy | Accessibility