Book An Appointment
Physician Assistants
Physical & Occupational Therapists
KneeMRI ScansNon-OperativePhysiatry
Physical Therapy
Podiatry
Spine
Sports Medicine
TraumaUrgent Care
X-Ray Imaging

Whether you’re just trying to stay active, chasing after your kids, or if it's your teen pushing through practices and games, shin splints can stop you in your tracks. That aching, sometimes sharp pain along the front of the leg isn’t only for athletes running marathons, it’s surprisingly common in everyday life. Kids in fall sports like soccer, football, and cross-country often run into it, but parents and adults who spend long hours on their feet or squeeze in workouts can feel it too. What starts as a dull soreness after activity can quickly turn into a daily frustration, making simple things like walking, climbing stairs, or enjoying playtime harder than they should be. Shin splints don’t just interrupt sports; they interrupt life. This post explains what causes shin splints, how they feel, how we diagnose them, and practical steps you can take to feel better. We cover common triggers, home care, when to see a specialist, and what recovery usually looks like.

You’ll learn why shin splints happen, what symptoms to watch for, which everyday habits make them worse, and how we at Princeton Orthopaedic Associates approach treatment and recovery.
Shin splints is a common name for pain along the shin bone that starts with activity. Classic shin splints most commonly refer to medial tibial stress syndrome, or MTSS, which presents as a diffuse aching along the posteromedial, or inner, border of the lower tibia near the distal half of the shin. Persistent pain over the front of the shin is less typical for MTSS and may indicate a tibial stress fracture or exertional compartment syndrome, so those symptoms should be evaluated.
MTSS is not just simple surface inflammation. It sits on a bone stress continuum where repeated overload affects the tibial cortex and the periosteum, and traction from muscles such as the soleus and tibialis posterior contributes to symptoms. We keep explanations simple but want you to know the pain often reflects mechanical overload of bone and the tissues attached to it.
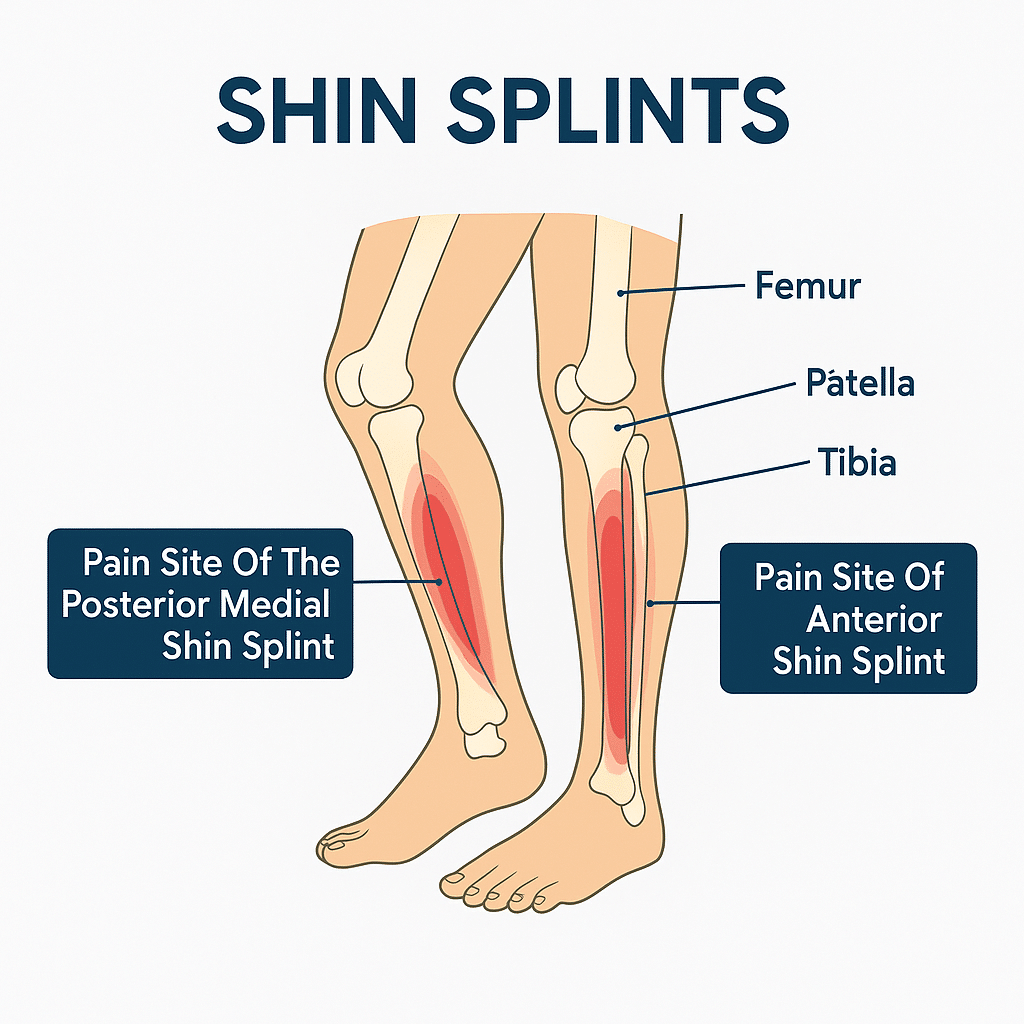
Symptoms of shin splints usually start as a dull, aching pain along the inner edge of the lower leg, often felt during activity and easing with rest early on. The pain typically covers a broader segment along the posteromedial tibia rather than a single sharp spot.
By contrast, a tibial stress fracture more often causes focal point tenderness, a small spot that is exquisitely painful to press. Exertional compartment syndrome may produce tightness, cramping, numbness, or weakness during activity. If your pain is sharp, highly localized, wakes you at night, or makes it hard to walk, see a clinician promptly to check for these possibilities.
Shin splints come from repetitive stress on the lower leg. You don’t have to be a runner to get them; they happen with many forms of exercise and work that increase load on the shin.
Diagnosis starts with a careful history and a physical exam. We check the pattern of pain, how it changes with activity, and look at your foot and ankle mechanics. The exam helps distinguish shin splints from a focal stress fracture or from exertional compartment syndrome.
If needed, imaging can help rule out a stress fracture or other conditions when symptoms are severe, very focal, or not improving with appropriate rest. X-rays are often the first test but can be normal early on. If concern persists, an MRI is more sensitive and can confirm a bone stress injury.
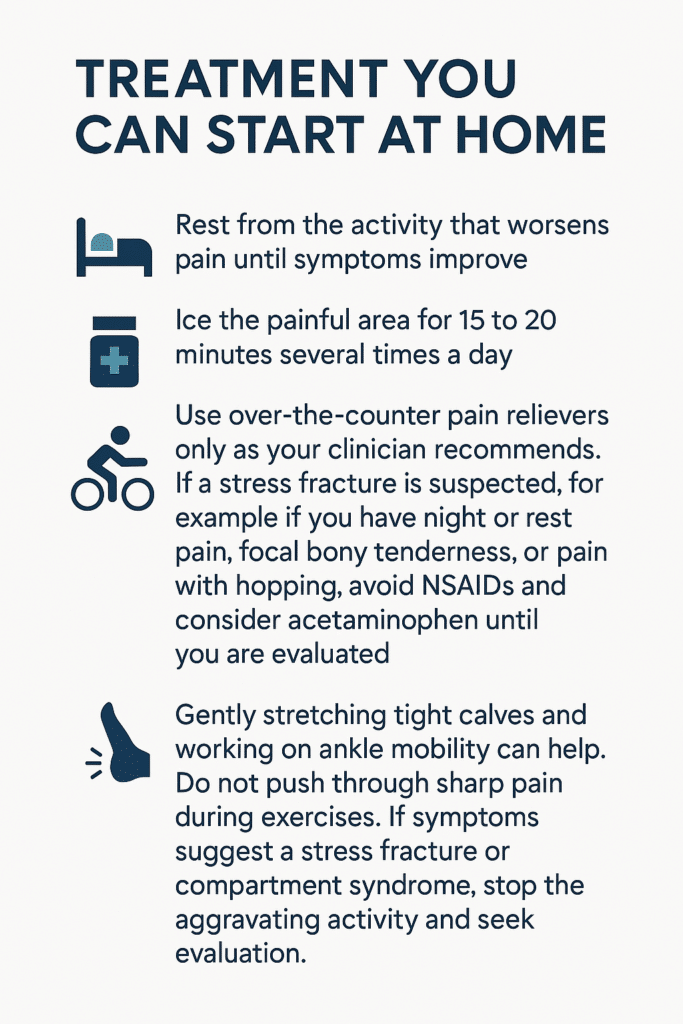
Gently stretching tight calves and working on ankle mobility can help. Do not push through sharp pain during exercises. If symptoms suggest a stress fracture or compartment syndrome, stop the aggravating activity and seek evaluation.
If symptoms persist, physical therapy is often the next step. A therapist will guide you through strengthening and flexibility work to correct the forces that stress the shin and help you return to activity safely.
Recovery time varies based on severity and how quickly you address the cause. The table below gives a general idea.
| Severity | Typical Recovery | Notes |
|---|---|---|
| Mild | 2 to 4 weeks | Relative rest, icing, and gradual return usually helps. |
| Moderate | 4 to 8 weeks | Often needs formal rehab and footwear changes. |
| Severe or Persistent | 8 weeks or more | May require imaging and a structured rehab plan to avoid stress fracture risk. |
Seek care if pain is severe, gets worse despite rest, or you cannot put weight on the leg. Also see a clinician if pain wakes you at night, if you have marked swelling, or if you have new numbness or weakness.
Be alert for signs that need prompt or urgent evaluation, including:
| Specialty | Why You'd See Them | Notes |
|---|---|---|
| Sports Medicine | Non-surgical diagnosis and treatment of overuse injuries | Good first stop for activity-related shin pain |
| Physical Therapy | Guided rehabilitation and return-to-activity plans | Focuses on strength, flexibility, and movement patterns |
| Foot and Ankle Specialist | When foot mechanics, orthotics, or surgical options are considered | Helpful if foot structure contributes to repeat problems |
Return to activity should be gradual and guided by pain. Increase load slowly and stop if symptoms flare. A simple progression to consider is pain-free walking, then a pain-free single-leg hop, then light jogging. If those steps are comfortable, gradually increase duration and intensity while continuing strengthening and mobility work.
If you are unsure whether your pain is caused by shin splints or something more serious, schedule an exam so we can check you and recommend the right next steps.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
You don’t have to be a marathon runner to feel that nagging ache on the outside of your knee. The important thing? It might not actually be your knee. It might be a tight IT band, and unlike joint injuries, it requires a different kind of treatment focused on mobility and muscle balance.
Maybe it starts during your daily walk, or when you’re going up stairs. Perhaps it flares up when you get up from your desk or out of the car. It might even wake you up at night, pulsing in your outer thigh or hip, making it impossible to get comfortable. It doesn’t feel like an injury yet, the pain keeps coming back.
If this sounds familiar, there’s a good chance your iliotibial band (IT band) is involved. And the condition you might be dealing with is called IT Band Syndrome, a common cause of outer knee and hip pain that affects far more than just athletes.
Let’s walk through what’s happening in your body, why it hurts, and most importantly, what you can do to start feeling better.
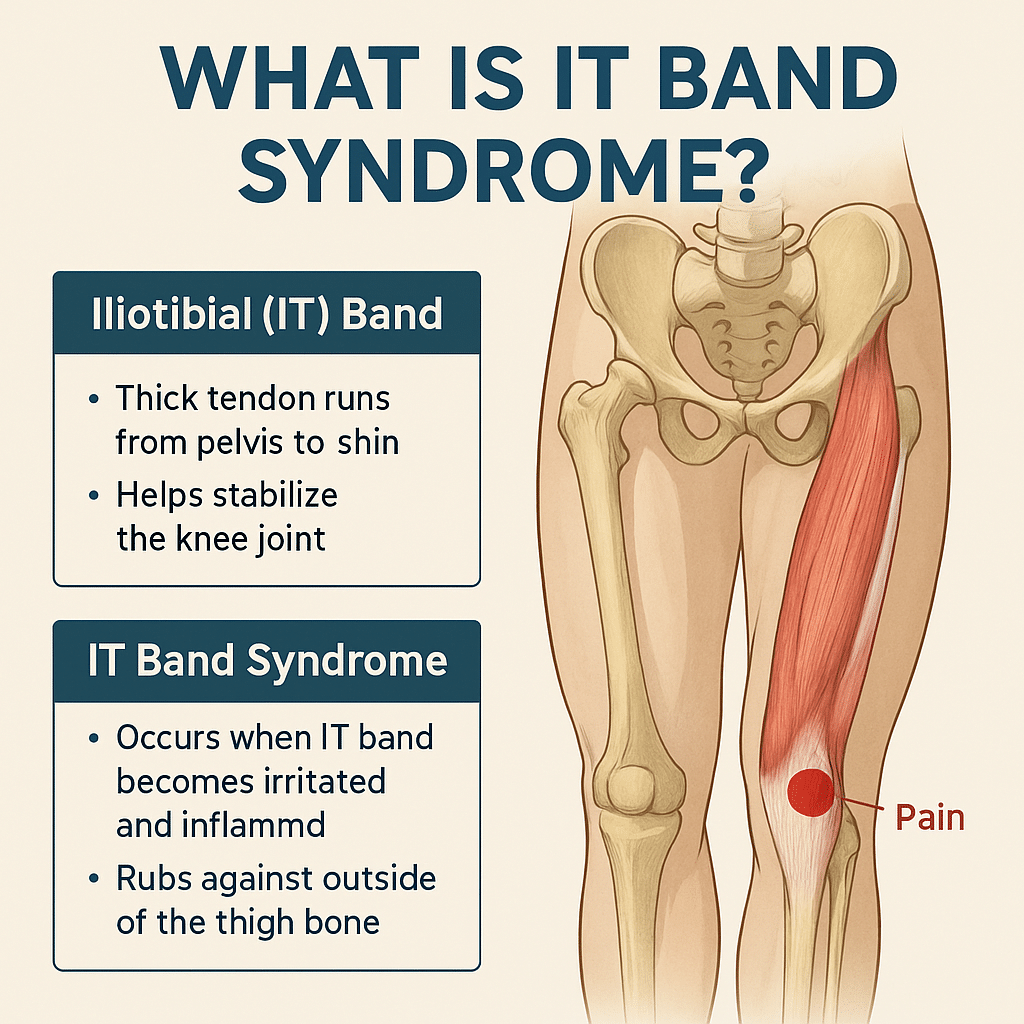
The iliotibial (IT) band is a thick, fibrous band of connective tissue that runs down the outside of your leg, from your hip to just below your knee. Think of it as a support strap that helps stabilize your knee and assist with hip movement.
When the IT band gets too tight, often due to repetitive movement, muscle imbalances, or poor posture, it can rub against the bone at the outer knee. This creates irritation, inflammation, and pain, commonly known as IT Band Syndrome (ITBS).
And while it’s often associated with athletes, it’s just as common in walkers, desk workers, parents, nurses, retail workers, and anyone who’s on their feet a lot, or not enough.
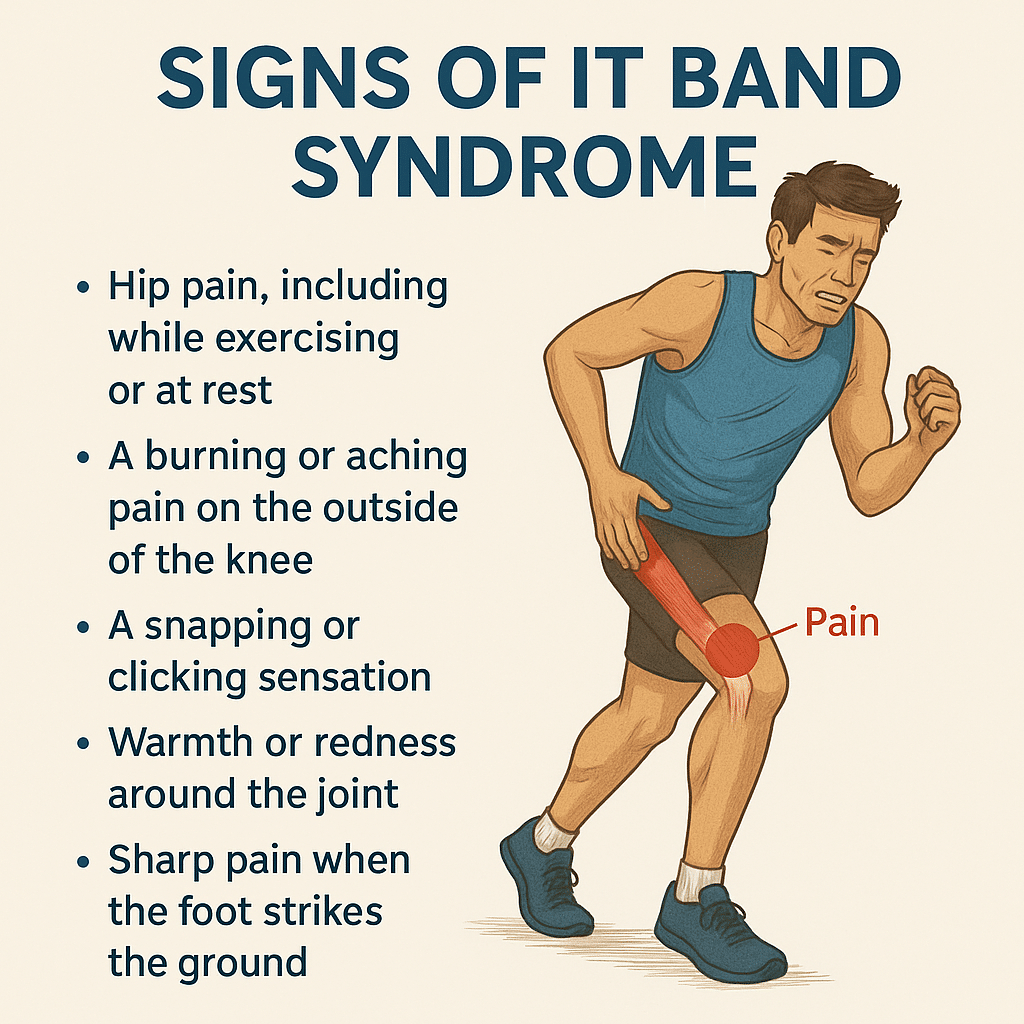
Here are common, real-world symptoms of IT Band Syndrome in everyday life:
These symptoms often start mild, but become more consistent if left unaddressed.
Even without intense training, everyday habits can contribute to ITBS:
While the core problem is the same (tightness and friction along the IT band), athletes often develop ITBS due to training volume and biomechanics. Common athletic triggers include:
IT Band Syndrome is common among:
💡Tip for athletes:
Strengthen your hips and glutes, cross-train, and make sure your recovery matches your training load
.
The IT band isn’t a muscle, it’s actually connective tissue. That means:
Over time, the friction and inflammation can become chronic and much harder to treat.
Treatment focuses on reducing inflammation, improving mobility, and correcting muscle imbalances.
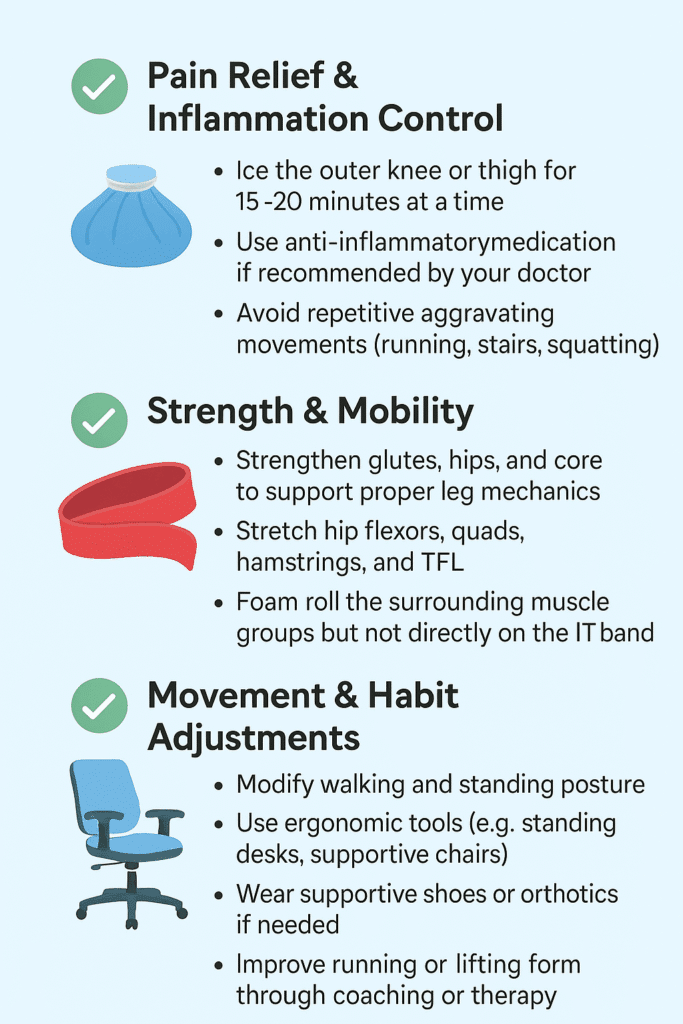
✅ Pain Relief & Inflammation Control
The length of time to recover from IT Band Syndrome depends on how long you've had symptoms and whether you're treating the root cause:
2-3 Weeks
Rest and stretching may help quickly if caught early
4-6 Weeks
Requires active rehab including movement correction
2+ Months
Long-standing tightness or inflammation takes time to unwind
IT Band Syndrome doesn't just show up during workouts; it can quietly interfere with our daily routine, mobility, and overall comfort. Without treatment, ITBS can impact your:
And for athletes, it can put your training on pause or create a cycle of recurring injuries.
If you have been experiencing symptoms of IT Band Syndrome and you haven't found relief, you should consult with a specialist. Especially if:
At Princeton Orthopaedic Associates, we have physicians from multiple specialties that can help you get to the root of your tight IT band and help set you off on the path to recovery.
-Trained to treat soft tissue overuse injuries like ITBS
- Can differentiate between joint issues and soft tissue problems
- Often the best first stop for a non-surgical, comprehensive evaluation
- Focuses on functional movement and musculoskeletal pain
- Great at managing chronic pain or postural imbalances
-Ideal for cases involving compensations, gait issues, or mobility problems
- Best if ITBS has persisted or if you need advanced imaging or diagnostics
- Also helpful if you suspect other structural issues like meniscus, arthritis, or leg length discrepancy
- A physical therapist is often the next step after diagnosis for hands-on treatment and long-term recovery.
Our specialists will identify the root cause of your tightness, guide you through targeted corrective exercises, and help you improve how you move—not just mask the symptoms.
Whether you're training for a race or just trying to get through the workday without pain, IT Band Syndrome can be disruptive, but it's absolutely treatable. The key isn’t just stretching or resting, it's understanding why the IT band is tight and retraining your body to move in a healthier, more balanced way.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
© 2025 Princeton Orthopaedic Associates. The contents of PrincetonOrthopaedic.com are licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. Copying without permission is strictly forbidden. Privacy Policy | Accessibility