Book An Appointment
Physician Assistants
Physical & Occupational Therapists
KneeMRI ScansNon-OperativePhysiatry
Physical Therapy
Podiatry
Spine
Sports Medicine
TraumaUrgent Care
X-Ray Imaging


Submitted by Jennifer Hasan, DPM
Nervous excitement is the best way to describe the rush of emotions that I felt in October 2024 after accepting an invitation by the organization Friends of Yimbo (FOY) to join their humanitarian trip to Kenya in June 2025. My purpose was to provide podiatric medical care in Yimbo, an underserved village in the western part of Kenya.
FOY is a charitable organization devoted to educating and empowering populations in and around Yimbo. The organization was founded in 2007 by brothers Charles and Ben Odipo to carry on the legacy of their father Joseph Odipo. He was a visionary who founded the Muguna Primary School, the first in the region. What began as a single classroom built by villagers is now a thriving school with 470 students and 10 classrooms. In addition to education, FOY initiatives also include access to clean water, community health, and economic development.
I was introduced to Charles and Ben by a colleague, Dr. Maria Sopchede, who participated in the humanitarian trip in 2024 and inspired me to participate in 2025. Approximately every other year FOY organizes a 12–15-day humanitarian trip to the village of Muguna in western Kenya. The trip is considered to be rugged and rustic but it is also an opportunity to see and experience the side of Kenya that tourists don’t get to see.
The eight months of preparation for the trip involved countless phone calls, emails, texts, and Zoom meetings with the Odipo family, medical authorities in Kenya, and the travelers. Medical supplies were ordered, vaccines were administered, Kenyan and Ugandan visas were obtained, trip insurance was purchased, and flights were booked.
Finally, the day came on June 21 to board the 14-hour flight from New York to Nairobi and meet up with the other 13 volunteers who came from California and Canada.
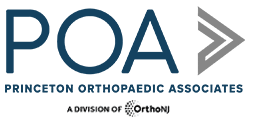
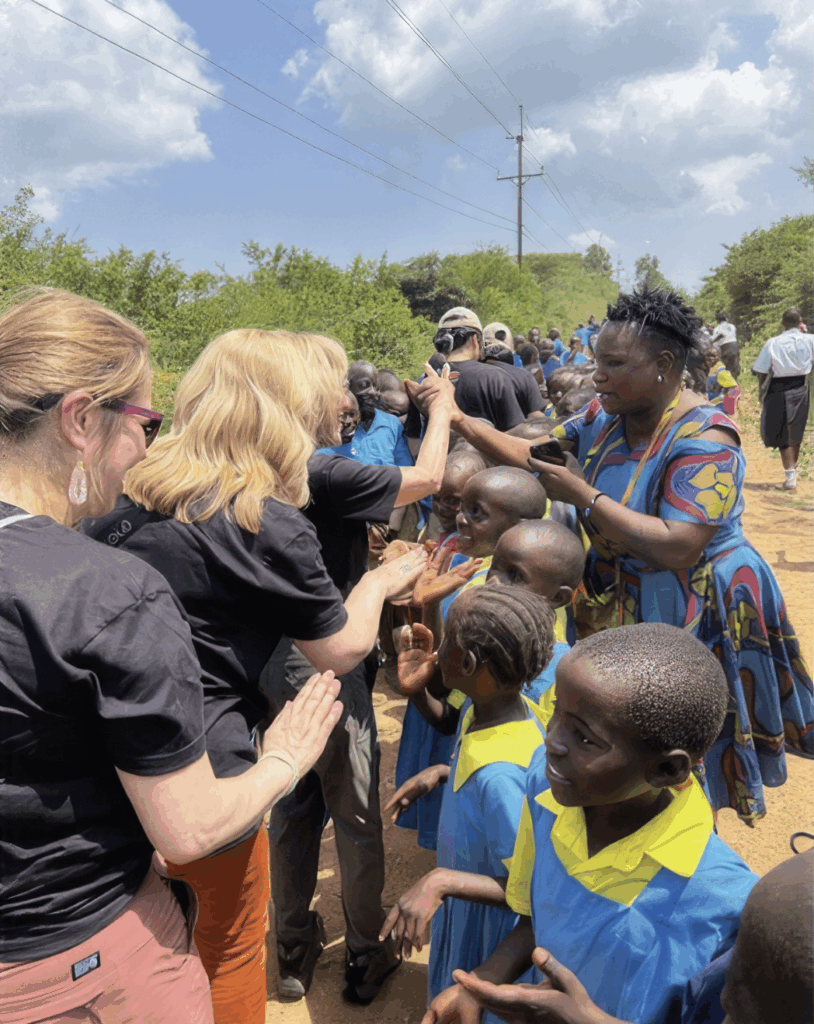
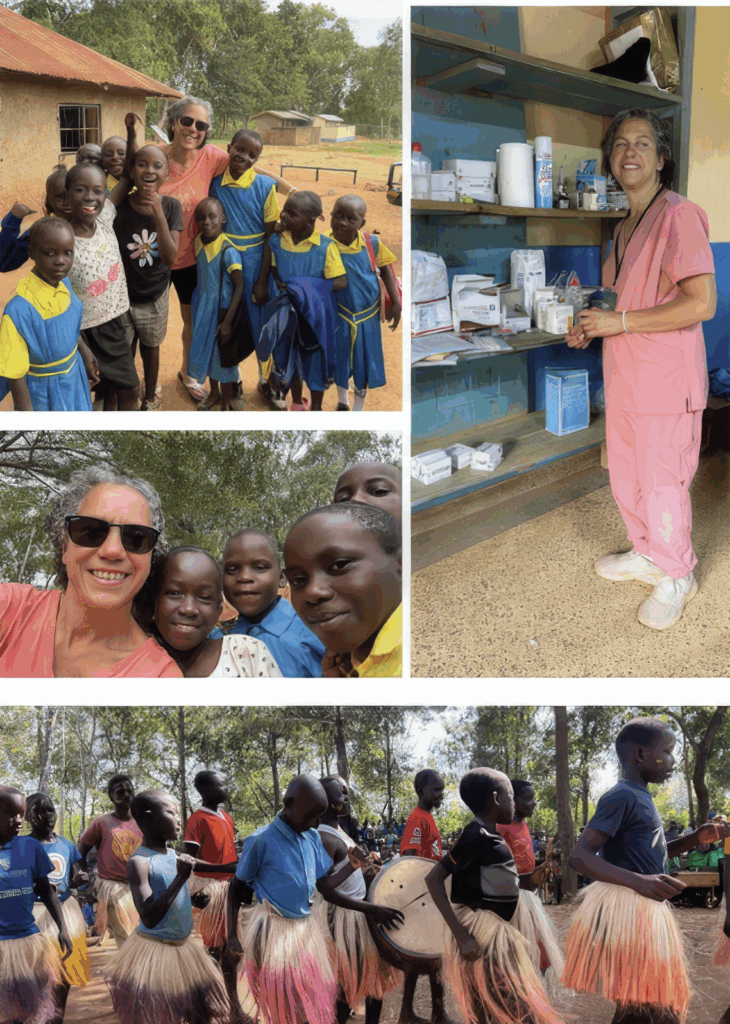
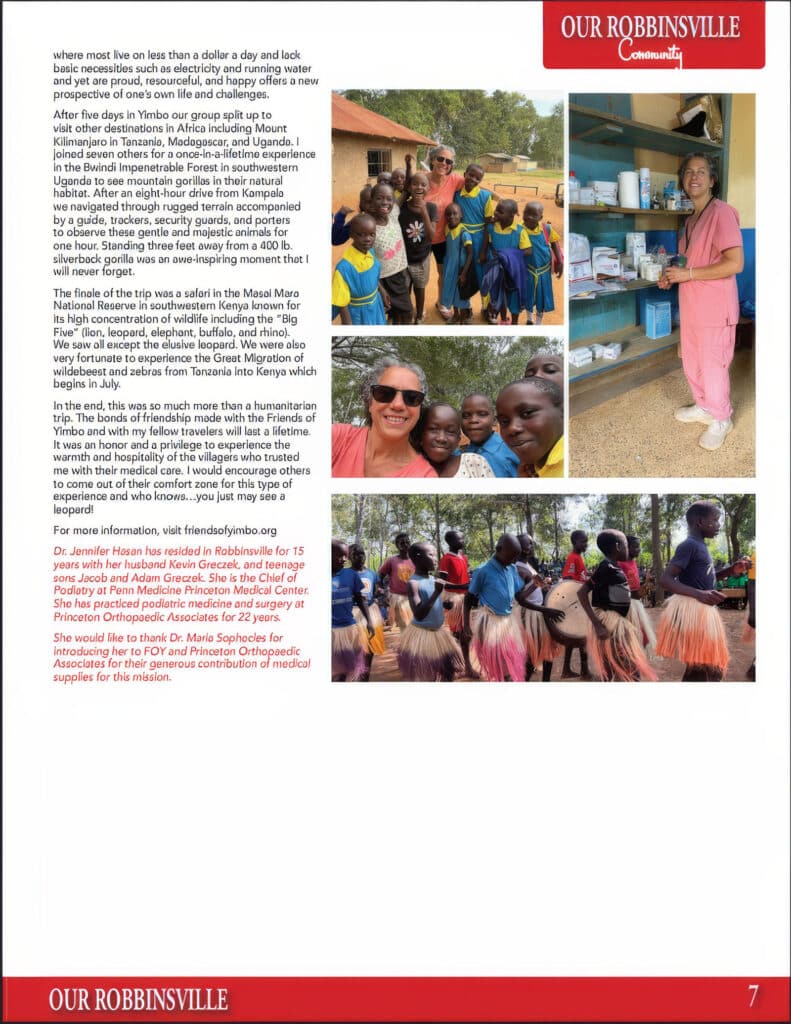
Upon arrival in the village, we were met by several hundred students, teachers, faculty, and community members and treated to a program of speeches, presentations, and traditional dance. The medical camp took place over three days in several basic classrooms within small enclosures in the Muguna School. Two hundred seventy-eight patients were seen, including 80 podiatry patients. The patients were largely impoverished and presented with a variety of conditions ranging from acute and chronic wounds, congenital deformities, and infectious diseases.
The patients were gentle and kind. Many walked or rode moped taxis for several miles to be treated at the medical camp and I was humbled by their strength, resilience, and patience. To spend time in a community where most live on less than a dollar a day and lack basic necessities such as electricity and running water and yet are proud, resourceful, and happy offers a new perspective of one’s own life and challenges.
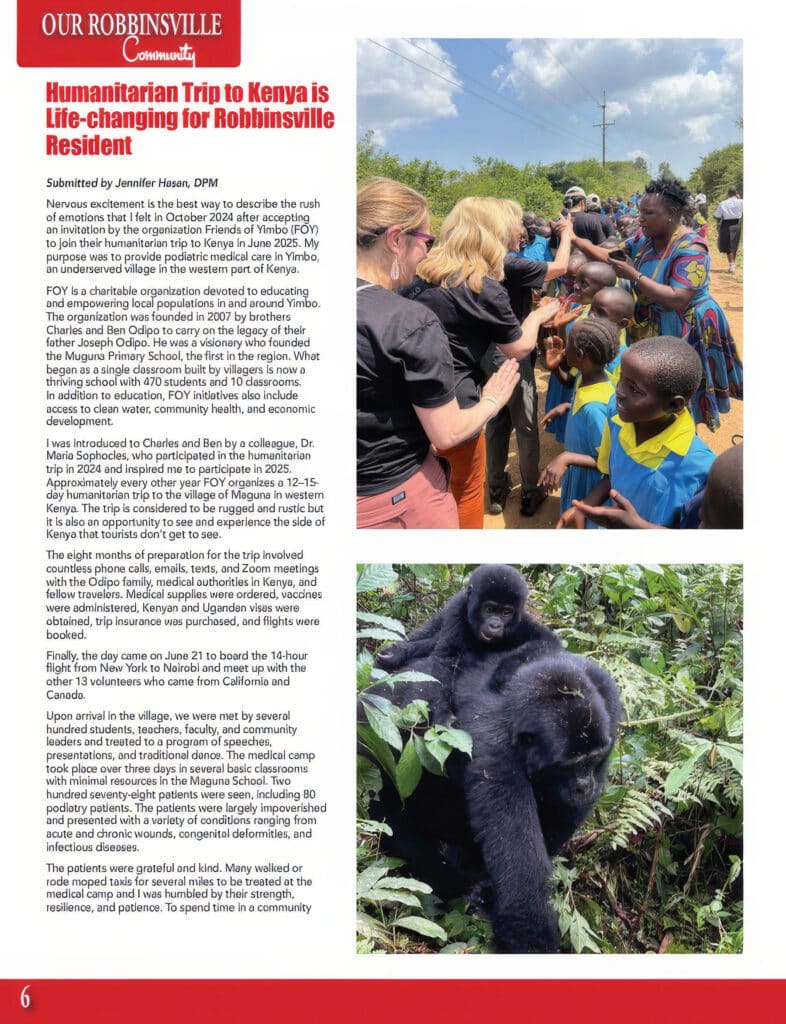
After five days in Yimbo our group split up to visit other destinations in Africa including Mount Kilimanjaro in Tanzania, Madagascar, and Uganda. I joined seven others for a once-in-a-lifetime experience in the Bwindi Impenetrable Forest in southwestern Uganda to see mountain gorillas in their natural habitat. After an eight-hour drive from Kampala we navigated through rugged terrain accompanied by a guide, trackers, security guards and porters to observe these gentle and majestic animals for one hour. Standing three feet away from a 400 lb. silverback gorilla was awe-inspiring moment that I will never forget.
The finale of the trip was a safari in the Masai Mara National Reserve in southwestern Kenya known for its high concentration of wildlife including the “Big Five” (lion, leopard, elephant, buffalo, and rhino). We saw all except the elusive leopard. We were also able to experience the Great Migration of wildebeests and zebras from Tanzania into Kenya which begins in July.
In the end, this was so much more than a humanitarian trip. The bonds of friendship made within the Friends of Yimbo and with my fellow travelers will last a lifetime. It was an honor and a privilege to experience the warmth and hospitality of the villagers who trusted me with their medical care. I would encourage others to come out of their comfort zone for this type of experience—and who knows…you just may see a leopard!
For more information, visit friendsofyimbo.org
Dr. Jennifer Hasan has resided in Robbinsville for 15 years with her husband Kevin Greczek, and teenage sons Jacob and Adam Greczek. She is the Chief of Podiatry at Penn Medicine Princeton Medical Center. She has practiced podiatric medicine and surgery at Princeton Orthopaedic Associates for 22 years.
She would like to thank Dr. Maria Sophocles for introducing her to FOY and Princeton Orthopaedic Associates for their generous contribution of medical supplies for this mission.
Good posture means your head, shoulders, and hips line up with your spine. This helps your body work well and move with less pain. Small, steady changes can add up over days and weeks. This guide explains why posture matters, common reasons it slips, safe exercises, and quick ergonomic setup ideas you can use at home or work to feel better and move more easily.

Good posture helps distribute forces evenly across your joints and muscles. When posture is poor, some muscles take on extra work while other areas weaken, which can lead to neck, shoulder, or back pain. The encouraging part is that steady, small changes usually lead to meaningful improvements.

Good posture means your head, shoulders, and hips line up so your spine is supported and muscles can work efficiently. It doesn’t mean you must sit perfectly rigid. Instead, aim for balance: a neutral spine with relaxed shoulders and an engaged core.
When your posture is balanced, less stress sits on joints and soft tissues, and you’re less likely to develop pain from overuse or compensatory movement patterns.
Posture affects pain, breathing, and how you move. Slouching can make neck and upper back muscles work harder. It can also change how your shoulders and hips move, which may lead to recent or gradual pain.
These choices are low-risk and can be done at home. Start gently and increase repetitions over weeks as you feel stronger. Evidence from major guidelines supports regular practice, with adults typically performing strengthening 2 to 3 days per week and stretches held for 20 to 30 seconds, gradually increasing as tolerated. (ACSM guidelines 2023)

People improve at different speeds. Small changes can show up in a few weeks if you practice regularly. Bigger, longer standing posture problems take longer to improve and may need a tailored plan. A steady mix of simple strengthening moves, daily posture habits, and help from a clinician or physical therapist can help you move better and reduce pain.
| Issue | Typical time to notice change | Notes |
|---|---|---|
| Minor slouching | 2 6 weeks | Daily breaks and basic exercises usually help. |
| Moderate postural imbalance | 4 6 weeks | Requires consistent strengthening and ergonomic changes. |
| Long-standing posture-related pain | 2+ months | Often needs a tailored program from a clinician or physical therapist. |
Try the self-care tips for a week or two. See a specialist sooner if pain limits your daily activities, if you change how you walk or move to avoid pain, or if home measures don’t help.
| Provider | What they help with |
|---|---|
| Primary care or sports medicine | Initial evaluation and recommendations for non-surgical care |
| Physical therapist | Hands-on treatment, personalized exercise programs, posture training |
| Physiatrist | Complex movement problems, chronic pain management, coordinate care |
At Princeton Orthopaedic Associates, we assess the root cause of posture problems and work with you to build a practical plan. We focus on restoring function and helping you return to activities with less pain.
If you need help customizing a program or you have persistent pain, schedule an exam so we can evaluate you and design a specific plan.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Gout is a common type of inflammatory arthritis that causes sudden, intense joint pain and swelling. In this guide, you will learn what gout is, why it happens, who is at higher risk, how we diagnose it, and the treatments that help you feel better and prevent future flares.

Gout happens when uric acid builds up in the blood and forms needle-like crystals inside a joint. Your immune system reacts to those crystals, which triggers sudden pain, redness, heat, and swelling. The big toe is the classic spot, but gout can affect the midfoot, ankle, knee, wrist, fingers, and elbow.
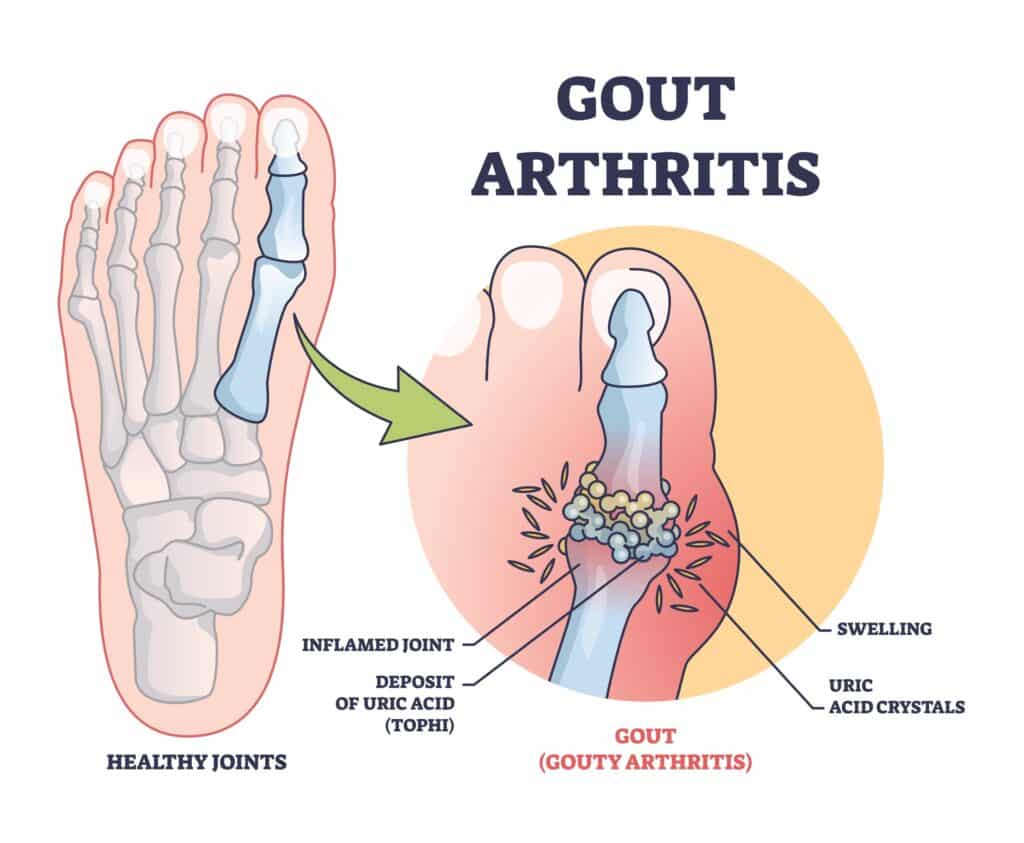
Uric acid forms when your body breaks down purines, which are found naturally in your tissues and in certain foods. When production is high or your kidneys don’t clear enough uric acid, crystals can deposit in joints and surrounding tissues. Cold areas like the big toe are common sites for crystal formation.
If you notice a new hot, swollen joint or have repeated gout flares, seek care promptly from a clinician or urgent care provider. Early evaluation helps confirm that gout is the cause, guides fast pain relief, prevents infection or other problems, and protects the joint from lasting damage. A clinician will review your health history and medicines to choose safe, effective treatment and avoid drug interactions.
During your visit, a clinician will look at the painful joint and review your overall health, symptoms, and medicines. The best way to confirm gout is to take a tiny sample of joint fluid and check it under a microscope for uric acid crystals. This test helps rule out infection and other problems that can look like gout.
Flares respond best when treatment starts early. The main goal is to ease pain quickly, reduce swelling, and lower inflammation while protecting the affected joint from more harm. Your doctor will tailor medicines to your health history and current medicines to ensure safety and effectiveness and help you return to daily activities.
Do not stop your long-term urate-lowering medicine during a flare unless your doctor advises it. Let us know at the first sign of a flare so we can tailor treatment to your health history and medications.
If you have repeated flares, tophi, kidney stones from uric acid, or moderate to advanced chronic kidney disease, you may benefit from urate-lowering therapy. The aim is to keep your blood uric acid below target so crystals dissolve and flares fade over time.
| Topic | Key Points |
|---|---|
| Who Should Start Urate-Lowering Therapy | 2 or more flares per year, tophi, uric acid kidney stones, or chronic kidney disease stage 3 or higher |
| First-Line Medicine | Allopurinol is typically first choice. Start low and increase gradually. Febuxostat is another option if needed. In patients with established cardiovascular disease, febuxostat carries an FDA boxed warning for increased risk of cardiovascular death. Use only after shared decision-making, and consider allopurinol first. Allopurinol can rarely cause severe cutaneous adverse reactions. Consider HLA-B*58:01 testing in high-risk groups (e.g., Han Chinese, Thai, Korean patients with CKD, and African American patients) before starting therapy. |
| Other Options | Probenecid may help if kidney function is adequate. Pegloticase is reserved for severe, refractory cases. Less effective with moderate-to-severe CKD; avoid or use cautiously in patients with a history of uric acid kidney stones; review for drug–drug interactions. |
| Target Uric Acid | Under 6 mg/dL is the usual goal. Under 5 mg/dL may be used if tophi are present. |
| Flare Prevention When Starting Therapy | Low-dose colchicine or an NSAID is often used for several months to reduce flare risk during dose adjustments. |
Our team evaluates the painful joint, confirms the diagnosis, and builds a treatment plan that eases pain fast and prevents future attacks. When appropriate, we can perform joint aspiration or an image-guided injection and coordinate long-term urate-lowering therapy with your broader care team.
If you think you're having a gout flare or you've had recurrent attacks, schedule an evaluation. Getting ahead of flares now helps protect your joints for the long term.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Understand what a meniscus tear is, the symptoms to watch for, how it’s diagnosed, and available treatment options. Learn when it’s best to see a specialist and what recovery typically involves so you can make informed decisions about your knee health.

A torn meniscus is a common knee injury that affects the cartilage pads that cushion your thigh bone and shin bone. You may get one from twisting your knee during sports or from gradual wear as you get older. Symptoms and treatments vary, and we walk through what you can expect at each step.
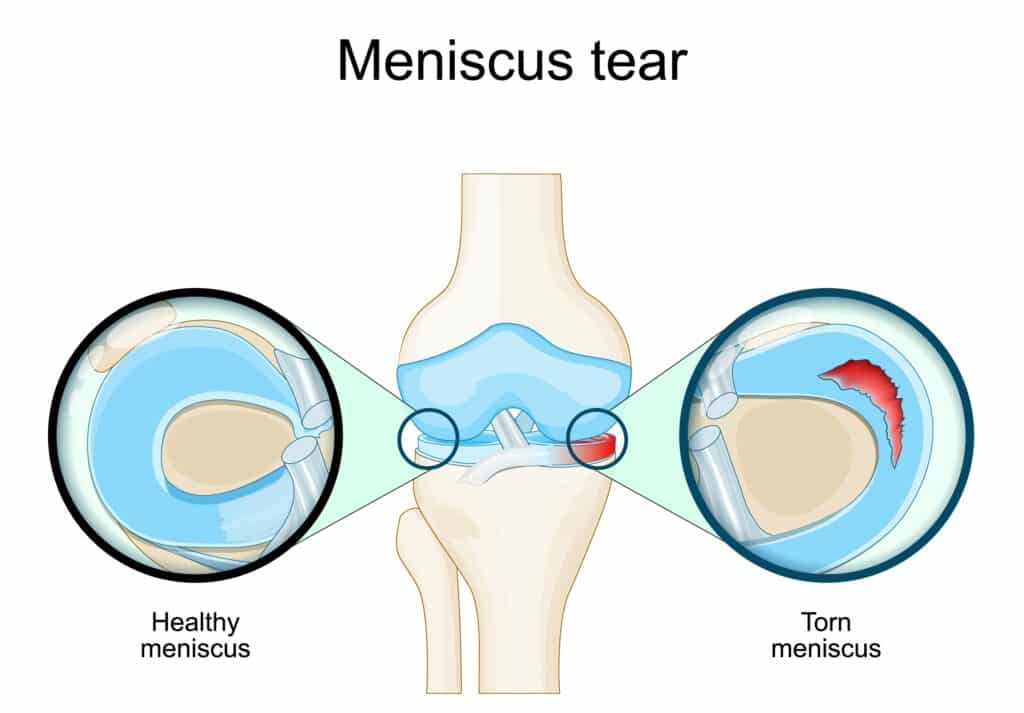
The menisci are rubbery wedges of cartilage that sit between your femur and tibia. They help spread load across the knee joint, absorb shock, and add stability when you twist or change direction.
When a meniscus tears, the knee loses some of that cushioning. That can cause pain with activity, swelling, and catching sensations. Over time, untreated problems can change how the joint wears, which may increase the risk of arthritis for some people.
Tears usually come from one of two patterns. Younger people often tear their meniscus during a forceful twist, pivot, or tackle. Older adults may develop a tear from gradual wear as the cartilage weakens with age.
We start with a focused history and knee exam. Certain exam maneuvers help us identify likely meniscal problems, and we check for swelling, range of motion, and mechanical symptoms.
If we need to confirm the diagnosis or plan treatment, imaging such as MRI is often helpful because it shows soft tissue details. X rays can rule out arthritis or bone issues.

Treatment depends on your symptoms, the tear type and location, your age, and your activity goals. We focus on relieving pain, restoring function, and protecting long term joint health.
If symptoms persist or there is a mechanical block in the knee, we may recommend arthroscopic surgery. Two common approaches are meniscal repair and partial meniscectomy.
Recovery varies based on the treatment chosen and the tear itself. Below are common timelines to help set expectations.
| Treatment | Usual Recovery | Notes |
|---|---|---|
| Conservative care | Several weeks to a few months | Many people improve with therapy and activity changes. |
| Partial meniscectomy | 4 to 8 weeks for many daily activities | Return to sports may be faster but depends on rehab and surgeon guidance. |
| Meniscal repair | 3 to 6 months | Requires protected rehab to allow healing of the repaired tissue. |
| Specialty | When to Choose | Role |
|---|---|---|
| Sports Medicine | Acute injuries and nonoperative care | Diagnosis, rehab planning, and nonsurgical management |
| Orthopedic Surgeon (Knee) | Persistent symptoms or mechanical problems | Discuss surgical options and perform arthroscopy when needed |
| Physical Therapy | Recovery after injury or surgery | Hands on care and guided strengthening to restore function |
If you want help protecting your knee or recovering from a meniscus tear, schedule an exam with one of our specialists. We personalize care so you can get back to your life with confidence.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
© 2025 Princeton Orthopaedic Associates. The contents of PrincetonOrthopaedic.com are licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. Copying without permission is strictly forbidden. Privacy Policy | Accessibility