Book An Appointment
Physician Assistants
Physical & Occupational Therapists
KneeMRI ScansNon-OperativePhysiatry
Physical Therapy
Podiatry
Spine
Sports Medicine
TraumaUrgent Care
X-Ray Imaging


Often, it starts subtly. You might notice a small lump in the palm of your hand. It isn’t painful, but it's firm and a little odd. Then you start to notice you're struggling to lay your hand flat on a table, or your fingers don’t extend like they used to when you stretch. Gripping a steering wheel, shaking hands, or even putting gloves on begins to feel different. Over time, one or more of your fingers start to curl inward toward the palm. This is often how Dupuytren's Contracture begins. A subtle, creeping change that slowly starts to change your hand function and your daily routine.
Dupuytren's Contracture is a hand condition where the tissue beneath the skin of your palm thickens and tightens over time. This fibrous tissue, known as fascia, can form cords that pull one or more of your fingers into a bent position. Once a finger is bent, it may not straighten fully, limiting your ability to perform daily activities.
Dupuytren's Contracture most commonly effects the ring and little fingers and usually progresses slowly over months or even years. Though not typically painful, it can significantly impact your hand function and quality of life.
Symptoms of Dupuytren's Contracture tend to develop gradually. Many people don’t notice anything is wrong until the condition has significantly progressed.
The exact cause of Dupuytren's Contracture is still not fully understood, but several contributing factors are known. It seems to be a combination of genetic and environmental triggers that lead to the thickening of connective tissue in the hand.
Contributing factors for developing Dupuytren's Contracture:
Unfortunately, there is no guaranteed way to prevent Dupuytren's Contracture, especially if you have a strong genetic predisposition. However, managing certain lifestyle choices may help reduce the risk or delay its onset.
Yes, Dupuytren's Contracture is strongly linked to genetics. If you have a family history of the condition, you have a higher chance of developing it. It is often referred to as a hereditary condition, especially prevalent among those of Northern European ancestry.
This doesn’t mean you’re guaranteed to develop it, but you may want to keep an eye out for early signs and consult a healthcare provider if you notice symptoms.

While Dupuytren's Contracture cannot be cured entirely, several treatments and management strategies can help maintain hand function and slow progression.
When the condition begins to interfere with your hand function, more active treatments may be helpful. These treatments for Dupuytren's Contracture can range from minimally invasive procedures to surgery.
Surgery (fasciectomy): In more severe cases, the thickened tissue is surgically removed.
Needle aponeurotomy: A needle is used to break the cords of tissue causing finger contraction.
Enzyme injections (collagenase): An enzyme is injected to soften and break down the cords.
Several factors may accelerate the progression or severity of Dupuytren's Contracture. Understanding these can help you avoid worsening the condition.
Overuse or certain jobs have not been definitively proven to cause Dupuytren’s Contracture. While it might seem like repetitive hand use or manual labor is the culprit (especially because many people who do physical work notice the symptoms), research hasn’t confirmed a direct cause-and-effect link.
Some people used to think Dupuytren’s Contracture was mostly a problem for manual laborers because of things like hand strain or using vibrating tools. But more recent research shows it can affect anyone, no matter what kind of job they have, even people who work at desks all day. Physical work might make the symptoms show up sooner, but it doesn’t actually cause the condition. If anything, overusing your hands once Dupuytren’s has started might make it worse, but it’s not the root cause.
Making practical adjustments to your daily activities can help you maintain your independence and comfort as you manage Dupuytren's Contracture.
If you notice any signs of finger contracture or thickened tissuein your palm, you should see a hand specialist. Early diagnosis can lead to better treatment outcomes.
Signs it’s time to see a specialist:
Diagnosis usually involves a physical examination. An orthopaedic hand specialist will assess the flexibility of your fingers and look for nodules or cords in the palm.
What the evaluation includes:
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
Yes, while there is no cure, Dupuytren's Contracture is treatable. With appropriate care, many people regain much of their hand function or prevent further deterioration. Early intervention is often key.
Treatment outcomes vary based on the severity of the condition and the method used. Some treatments offer lasting relief, while others may need to be repeated.
Living with Dupuytren's Contracture can be manageable with awareness and timely care. Many people continue to live active, fulfilling lives with the help of therapy, medical treatments, and modifications. Emerging therapies and surgical techniques continue to improve outcomes.
Stay informed, stay proactive, and don’t hesitate to seek help when changes begin.
Avoiding certain actions can help prevent further damage or worsening of the condition.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
At Princeton Orthopaedic Associates, your journey to better mobility and less pain doesn't end at the clinic doors. We’re thrilled to now offer Prescribe FIT, an innovative, insurance-covered virtual health coaching program that brings real, lasting change right to your home.
Whether you’re preparing for surgery, recovering from one, or simply hoping to reduce joint pain and improve your lifestyle, Prescribe FIT was made with you in mind.
Prescribe FIT is more than just a health coaching program; it’s a partnership. You are paired with your own dedicated health coach, who works one-on-one with you to support healthier eating habits, consistent physical activity, and other simple lifestyle changes that can have a significant impact on orthopedic health.
This isn’t a one-size-fits-all solution. Your health coach will tailor each step to your unique goals, challenges, and daily routines, helping you stay motivated, on track, and supported every step of the way.
Musculoskeletal (MSK) conditions like osteoarthritis, back pain, joint injuries, and post-surgical recovery are deeply affected by lifestyle habits. For many patients, weight loss and increased mobility are essential to reducing joint stress and chronic discomfort.
With Prescribe FIT, you can:
And the best part? You do it all from the comfort of your home, with expert support just a phone call or message away.
We believe that better health should be accessible to everyone. That’s why Prescribe FIT is covered by Medicare, Medicaid, and most major commercial insurers. Our friendly POA team will help you verify your eligibility and explain any financial responsibilities up front, so you can focus on your health, not the paperwork.
If you’ve been told weight loss or lifestyle changes could help your orthopedic condition, but you’re unsure where to start, Prescribe FIT is the perfect place. There’s no pressure, no crash diets, no complicated gym routines. Just real, achievable goals that help you feel better, move better, and live better.
At POA, we’re always looking for ways to expand your care beyond the exam room. Prescribe FIT is one more way we’re investing in your long-term wellness, because how you heal matters just as much as where you heal.
Ask your POA provider about Prescribe FIT at your next visit, or contact us today to learn more about enrollment.
Let’s take the first step, together.
An ACL tear typically occurs during sudden pivoting, awkward landings, or stops, which are common in sports such as basketball, soccer, and skiing. It usually starts with a moment, an awkward pivot during a pickup basketball game, a sudden stop on the soccer field, or landing just slightly wrong after a jump. You might feel a sharp pain, instability, or hear that telltale pop. You go down, maybe hoping it’s nothing, but your knee swells, and walking becomes difficult. That’s the moment many athletes, professional, weekend warriors, or even teenagers, begin their journey with an ACL tear.
Understanding how to recognize a minor knee issue needing minimal home treatment versus what may be an ACL tear can be critical to the proper treatment and the fastest path to healing.
Your knee is one of the most complex joints in your body, and the ACL is one of its most important components. It plays a huge role in keeping your knee stable and allowing you to move with confidence, whether you're sprinting down a field or simply walking downstairs.
The ACL (anterior cruciate ligament) is one of the four major ligaments in your knee, connecting your thigh bone (femur) to your shinbone (tibia). Its job is to stabilize the knee, especially during rotation, pivoting, and rapid direction changes. That makes it crucial for athletes, but also important for anyone who walks, runs, or climbs stairs.
When the ACL tears, it doesn’t heal on its own. And unlike muscles, ligaments don’t regenerate well without surgical reconstruction.
If you’ve injured your knee and are wondering if it’s your ACL, you’re not alone. Knowing what symptoms to look for can help you decide whether it’s time to see a doctor or get imaging.
Here’s what people often report:
Some people can walk after an ACL tear, especially once swelling subsides, but the knee often feels unstable. Grade 1 (mild) tears may feel like soreness and instability under stress, but they’re rare. By two weeks post-injury, swelling may reduce, but instability often persists.
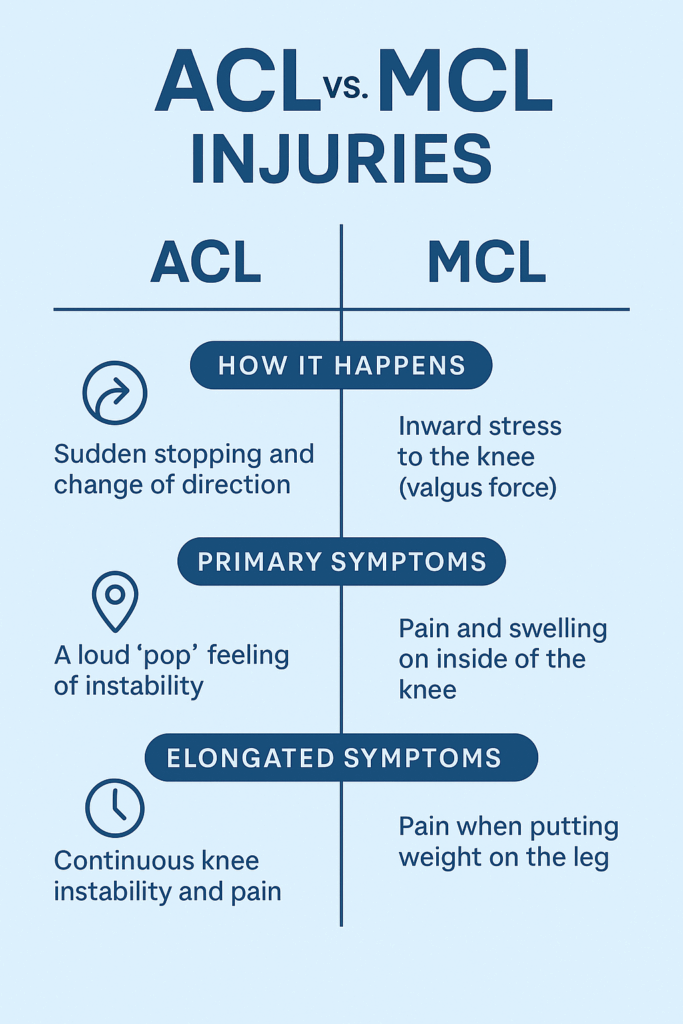
Knee injuries can be confusing because symptoms often overlap. The ACL and MCL are two different ligaments with different functions, injury mechanisms, and treatment approaches. Understanding the difference is critical for proper recovery.
Many people confuse ACL and MCL (medial collateral ligament) injuries. Here’s how an ACL tear and MCL tear differ:
| ACL Tear | MCL Tear | |
| Location | Inside the knee, central | Inside of the knee (medial side) |
| Mechanism | Pivoting, cutting, or landing | Direct blow to outer knee or overstretching |
| Sound | Often a pop | Less commonly a pop |
| Swelling | Fast and significant | Less severe swelling |
| Instability | Knee feels unstable or “gives out” | Usually more stiff than unstable |
| Healing Potential | Does not heal on its own | Often heals without surgery |
| First-line Treatment | Physical therapy or surgical reconstruction | Bracing, rest, and physical therapy |
| Surgery Needed? | Often required in active patients | Rarely required (unless Grade 3 + other injuries) |
| Return to Sport | 6–12 months (after reconstruction) | 4–12 weeks (depending on severity) |
Key difference: An MCL tear can often heal with rest and bracing. An ACL tear usually won’t.
Yes, and this is more common than people think, especially in sports injuries. This is called a combined ligament injury and often involves the ACL, MCL, and/or meniscus. These cases require specialized surgical planning and longer rehabilitation timelines, making early diagnosis even more critical.
While some clues (pain location, swelling speed, mechanism) may point toward one ligament over the other, you cannot reliably self-diagnose an ACL or MCL tear. Some people with a complete ACL tear are still able to walk or bend their knee, which can be misleading.
We recommend consulting one of our sports medicine specialists or an orthopedic knee surgeon as soon as possible. A timely and accurate diagnosis gives you the best chance of a full recovery and of avoiding chronic knee issues.
When it comes to ACL injuries, age matters. Kids and teens are still growing, and that can make treatment more complicated. What’s best for a 14-year-old soccer player may be very different from what’s recommended for a 30-year-old runner.
ACL injuries are increasing in adolescents, especially teenage athletes. The growth plates (areas of developing cartilage near the ends of long bones) in kids add complexity:
In adults, decisions are often based on lifestyle, activity level, and degree of instability.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
Surgery isn't always required for an ACL tear, but it can often be recommended. Once you’ve torn your ACL, the big question is: Do you need surgery? The answer depends on your goals, age, activity level, and the nature of the tear. For some, physical therapy may be enough. For others, reconstruction is the most straightforward path back to full function. Your treatment path is specific to you, and our specialists will build a plan that meets the needs of your injury and desired recovery outcome.
Mild (grade 1) sprains may recover within 3–6 weeks with rest and rehab.
For:
Approach:
Surgery may sound intimidating, but for many people, it offers the best chance at regaining full knee stability and returning to high-level physical activity. The procedure is common, safe, and continually improving.
Most active individuals, especially athletes or younger patients, choose ACL reconstruction. Here’s how it works:
Factors influencing surgery:
Sometimes what you don’t do is just as important as what you do. The wrong move after an ACL tear can worsen the injury or lead to complications down the line.
Leaving an ACL tear untreated can lead to further joint damage, including cartilage wear or meniscus tears.
Some people can still walk, squat, or bend their knee shortly after tearing their ACL. However, without stability, these motions can cause further injury. If you suspect you have an ACL tear we recommend you see a orthopaedic specialist as soon as possible for a comprehensive evaluation.
An ACL tear is a detour, not a dead end. With the right care, commitment, and patience, people of all ages get back to running, jumping, and playing, often even better than before.
Tearing your ACL can feel like the end of your athletic identity, but it’s not. Thousands of people, from high school athletes to weekend hikers to pro players, successfully return to sports and active lifestyles every year.
The key is getting the right diagnosis, choosing the right treatment path for your goals, and committing to smart, structured rehab.
While some symptoms can help differentiate between the two, it’s extremely difficult to diagnose knee ligament injuries accurately without imaging and specialist assessment.
Bottom Line: Always get a clinical evaluation with a knee specialist, especially if you heard a pop, felt instability, or have swelling. Don’t self-diagnose based on symptoms alone.
Tearing your ACL may feel overwhelming, but it's not the end of your active lifestyle. Whether you're a competitive athlete or someone who just wants to move without fear, recovery is possible with the right approach. From early diagnosis and personalized treatment plans to structured rehab and return-to-play timelines, every step forward matters. Understanding your options is the first step toward getting back to what you love, with strength and confidence.
If you’re reading this, you may be worried about what’s next. Take a breath, you’re not alone. Understanding your injury is the first step toward healing. Now it’s time to take action. If you suspect an ACL tear, don’t wait. Get evaluated by a sports medicine physician or orthopedic specialist. Early diagnosis means earlier healing and a better chance of getting back to doing what you love.
While both ACL and meniscus injuries are common in athletes and active individuals, they are very different in structure, symptoms, and recovery needs. Knowing the distinctions can help guide proper diagnosis and treatment.
| Symptom | ACL Tear | Meniscus Tear |
| Popping Sound | Very common | May occur, but less dramatic |
| Swelling | Rapid (within hours) | Gradual (over 24–48 hours) |
| Instability | Knee may "give out" | Usually feels stable |
| Pain Location | Deep or central knee | Side or back of knee (depending on tear location) |
| Mobility | Loss of motion due to swelling and instability | May still walk, but discomfort with twisting/squatting |
| Symptom | ACL Tear | Meniscus Tear |
| Knee Giving Out | Frequent instability, especially during pivoting | Rarely unstable |
| Locking or Catching | Uncommon | Very common — knee may catch or lock during motion |
| Grinding or Clicking | Occasionally | Common, especially with movement |
| Degeneration Risk | Higher if combined with meniscus injury | Increases risk of arthritis over time |
| Return to Activity | Difficult without surgery for active individuals | Sometimes possible without surgery, depending on severity and tear location |
A meniscus tear often presents with joint line tenderness and mechanical symptoms (like locking), while an ACL tear leads to feelings of instability and swelling shortly after injury. However, since both can coexist, and symptoms can overlap, accurate diagnosis with an MRI and specialist evaluation (by a POA or orthopedic physician) is essential. Read more about meniscus tears.
| ACL | Meniscus | |
| Function | Stabilizes the knee | Cushions and supports joint movement |
| Injury Type | Ligament | Cartilage |
| Instability? | Yes | Rarely |
| Locking | Rare | Common |
| Needs Surgery | Often (for active patients) | Sometimes, depending on tear type |
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
You were mid-pivot, chasing a ball or turning to grab something behind you, when a sharp pop hit your knee. Not loud, but distinct. You paused, unsure if it was serious. Maybe just a tweak, you thought. But within hours, the swelling crept in, the joint stiffened, and walking suddenly felt unfamiliar. That small twist? It turned into something much bigger.
That moment likely marked the beginning of a meniscus tear—a common yet disruptive injury affecting the cartilage in your knee. Whether it's from a sudden injury or years of wear and tear, the result is often the same: pain, limited movement, and questions about what comes next.

Inside each of your knees are two rubbery, wedge-shaped pieces of cartilage: the medial and lateral menisci. These act like shock absorbers between your thighbone and shinbone, helping to distribute weight and stabilize movement. A tear occurs when this cartilage is damaged—usually from twisting motions or degeneration over time.
You don't have to be an athlete for this to happen. A quick squat, an awkward turn, even standing up too fast with pressure on the joint can be enough, especially if the cartilage is already weakened with age.
There are two primary culprits behind a torn meniscus:
Both scenarios are incredibly common. Lifting a heavy box incorrectly or kneeling on a hard surface for too long can be all it takes.
The first few hours after the tear are often the most telling. At first, discomfort may be the only symptom of a meniscus tear you might feel. Or, the only symptoms of a meniscus tear present at first are just a dull, persistent ache, made worse by movement. You might feel fine while sitting, but as soon as you try to walk or bend, your knee doesn't cooperate. Some describe it as a "stuck" sensation, where the joint feels like it won't fully extend or flex without pain or resistance. But then the pain deepens, swelling begins, and your range of motion shrinks even more.
Clicking, popping, or catching during movement can also indicate a torn flap of cartilage catching in the joint. Check out this post to read more about the Types of Meniscus Tears.
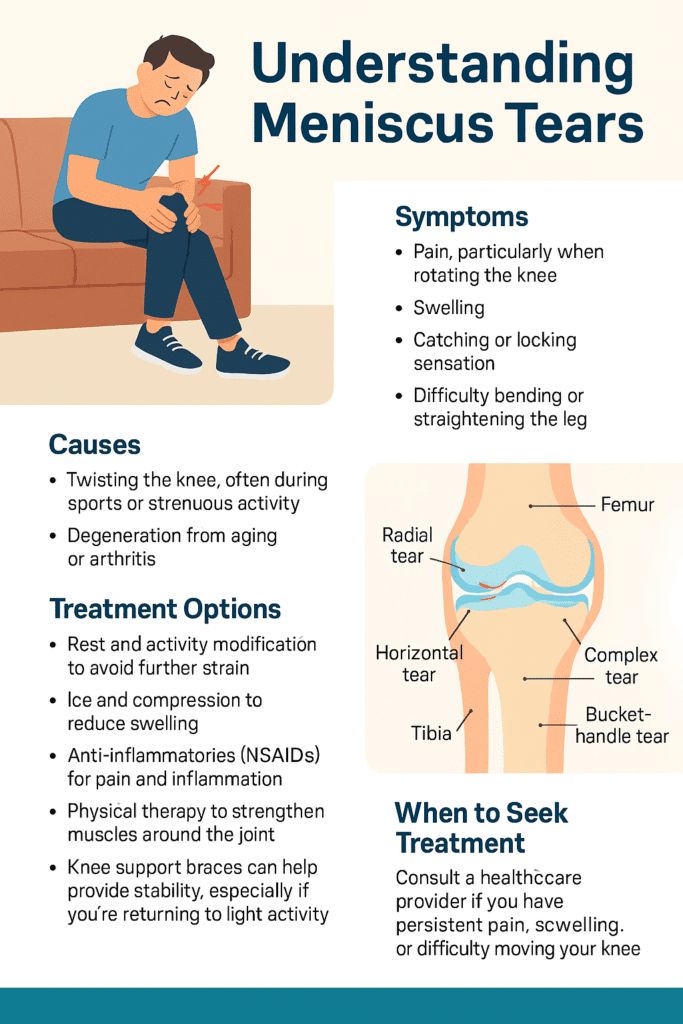
If you're looking for clarification on the symptoms of a meniscus tear, you are not alone. Many people deal with a torn meniscus and don't realize the seriousness until the stiffness and pain don't go away.
If you're hoping it will just go away, consider this: untreated meniscus tears can worsen over time, leading to more pain and even long-term joint issues like osteoarthritis.
Seek professional help if:
Ignoring it risks further tearing or cartilage breakdown. Early diagnosis often means better, less invasive treatment options.
A physical exam can often provide early clues. A clinician will test your range of motion and apply gentle pressure or rotation to identify pain points. In many cases, imaging, like an MRI, is used to confirm the diagnosis and pinpoint the severity and location of the tear.

Not all meniscus tears require surgery. If you're looking for a meniscus tear remedy, treatment depends on the type of tear, location, and severity of the tear, as well as your activity level and age.
Small tears near the outer edge, where the blood supply is richer, often heal with conservative care.
If the tear is large, causes locking, or doesn't improve, arthroscopic surgery may be recommended. Options include:
Surgery is more likely in younger, active individuals or when the tear is in a critical area.
How long it takes a torn meniscus to heal depends entirely on the treatment path and your consistency with rehab. Below is a general idea of recovery times based on the type of treatment - this is for reference only and not a diagnosis and treatment.
Conservative (rest, PT)
4-8 weeks
Partial Meniscectomy
4-6 weeks
Arthroscopic Repair
3-6 months
So, how long does it take for a meniscus tear to heal? It may take time to regain strength and trust in your knee even after healing.
Yes—but that doesn't mean you should. Many people are able to walk with a torn meniscus, especially if the pain is mild. But without proper treatment, walking on a torn meniscus can cause further damage or transform a minor tear into a more serious one.
If you must stay mobile, supportive bracing and avoiding twisting motions is essential.
Despite the pain and swelling, a torn meniscus often doesn't present visible signs like bruising or discoloration. That's why if you're looking for answers to "what does a torn meniscus look like on the outside," the truth is, it doesn't look like much so you won't find much. The damage is internal; symptoms often show through movement limitations and experienced pain, not appearance.
Prevention of a meniscus tear isn't just about avoiding sports injuries—it's about daily movement, posture, and support.
While it's no guarantee you'll avoid having a torn meniscus, there are some smart prevention strategies! Some strategies include:
You don't need to be an athlete to tear your meniscus—and you don't need to live with the pain either. Even activities like walking the dog or playing with your kids carry risk if you're not mindful of sudden directional changes! With awareness, early action, and proper care, recovery is possible and often complete. Pain-free movement starts with taking your symptoms seriously, getting the right diagnosis, and committing to healing fully.
If it feels wrong, it probably is. Trust your body, and give it what it needs to bounce back. Contact us today to schedule with one of our specialists.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.

You wake up in the morning and swing your legs over the edge of the bed. Before your feet even hit the floor, there it is—a deep, nagging tightness at the front of your hip. Walking to the kitchen feels stiff, almost like your legs are moving through molasses. You stretch instinctively, but it doesn’t quite hit the spot. When you sit down with your coffee, the ache creeps back in. Sitting at your desk later, the discomfort becomes sharp, pulling with every shift in position. Going for a jog—something that used to energize you—now leaves your hips feeling locked up, like rusty hinges refusing to swing open. This is life with tight hip flexors: a quiet, persistent thief of your freedom of movement.
For many adults, especially those with desk jobs or active lifestyles, hip pain can sneak in gradually and eventually become a daily discomfort. Having tight hip flexors is one of the most common culprits. Whether you spend hours sitting at a computer or you're constantly on the move, running or cycling, your hip flexors may be working overtime—and not always in a good way. Understanding how hip flexor tightness develops, and more importantly, how to alleviate it, is key to maintaining healthy, pain-free movement.
The hip flexors are a group of muscles located at the front of your hips that play a vital role in nearly every lower body movement. These muscles allow you to lift your knee toward your chest, bend at the waist, and stabilize your pelvis during standing, walking, and running.
The key muscles in the hip flexor group include:
These muscles work together to allow fluid motion, but when overworked or underused, they become shortened and tight, resulting in limited mobility and discomfort.
Hip flexor tightness often arises from a combination of inactivity and muscular imbalance, and in some cases, overuse.
Prolonged Sitting: Sitting for extended periods—at a desk, in a car, or on the couch—keeps the hip flexors in a shortened position. Over time, this leads to adaptive shortening and chronic tightness.
Repetitive Activity: Runners, cyclists, and athletes performing frequent leg lifts use their hip flexors intensively. Without adequate recovery and stretching, this overuse causes the muscles to become stiff and inflamed.
Muscle Weakness: Weakness in the glutes, deep core muscles, and stabilizers like the piriformis shifts the workload to the hip flexors, which are not designed to handle prolonged stabilization. This compensation pattern leads to over-recruitment and tightness.
Poor Posture or Pelvic Alignment: Anterior pelvic tilt (a common postural issue where the pelvis tilts forward) places the hip flexors in a shortened state even while standing.
When you have tght hip flexors it can reduce the range of motion in your hips, cause pelvic misalignment, and place strain on the lower back. You might feel discomfort in your groin, stiffness in the front of your hip, or even aching pain during or after activity. Long-term tightness can lead to:
If this issues is lefft unaddressed, this tightness becomes more than a nuisance to you—it becomes a chronic issue that impacts every step, sit, and stride.
Hip flexor pain is most commonly felt in the front of the hip and upper thigh, but it can also radiate to other nearby areas depending on the severity, cause, and specific muscles involved.
This is the most common location. It may feel like a deep ache or sharp pinch where your thigh meets your pelvis, especially when lifting your knee, walking uphill, or standing after sitting.
Pain can extend downward along the front of the thigh, particularly if the rectus femoris (a dual-function hip and knee flexor) is involved.
If the iliopsoas is especially tight or inflamed, pain may be felt deep in the inner hip or groin.
Because the psoas muscle attaches to the lumbar spine, chronic tightness or spasms can lead to referred pain or tension in the lower back.
Misalignment caused by tight hip flexors can lead to pain around the SI joints or pelvic rim.
In some cases, overuse of the rectus femoris can cause discomfort that tracks down toward the knee.
If the pain is sharp, persistent, or affects your ability to walk or move normally, it may be a sign of a strain, tendonitis, or labral issue—warranting a visit to an orthopedic specialist or physical therapy.
Prevention goes beyond stretching. It involves a comprehensive movement and strength strategy to ensure the hip flexors are neither overloaded nor neglected:
If you're already dealing with symptoms of tightness, there are ways you can find relief. It's beneficial to take a multi-pronged approach:
Hip flexor stretches done at home help restore flexibility and mobility in the front of the hips, reducing stiffness from prolonged sitting or repetitive activity. Regular stretching can alleviate pain, improve posture, and enhance movement efficiency during daily activities or workouts. Additionally, it supports pelvic alignment and reduces strain on the lower back by balancing muscle tension across the hip complex.

These evidence-based stretches are simple, safe, and effective. Perform them twice daily, holding each for 30–60 seconds per side, and repeat for 2–3 sets.
This stretch helps open the hip while promoting glute engagement.
Instructions:
Improves rotational mobility of the hip joint.
Instructions:
Uses gravity to gently open the hip flexors.
Instructions:
Targets both the front thigh and deeper hip structures.
Instructions:
While stretching and strengthening can resolve many cases of tightness, persistent or worsening pain should not be ignored. You should seek care if you experience:
The Right Specialist to See:
If you are experiencing persistent or worsening hip flexor pain like those just mentioned, it's important you see a specialist for an evaluation. At Princeton Orthopaedic Associates, we have multiple specialists who can help with your hip flexor pain. Contact us to schedule an appointment.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
Tight hip flexors don’t just affect how your hips feel—they influence your spine, posture, gait, and overall comfort. They can sideline your fitness, sap your energy, and even cause pain elsewhere in the body. Fortunately, with the right combination of movement, strengthening, and stretching, you can restore mobility and function to your hips. Don’t let tight muscles limit your life—take action early and seek professional care when needed.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Meniscus tears are classified based on tear shape and tear location. This classification helps determine whether the injury may heal with rest and therapy or if it needs surgical treatment. If you're looking to understand the type of tear you have, we have broken them down below:
A radial tear cuts straight across the meniscus from the inner edge toward the outer rim, similar to the spoke of a wheel. These are common and usually occur in areas with poor blood flow, which limits the body’s ability to heal the tear on its own. Treatment often involves trimming the damaged section.
A horizontal tear runs between the upper and lower layers of the meniscus, dividing it in half like a sandwich. These tears are more common in older adults and may be repairable if located in the outer region of the meniscus, where blood supply is better.
This tear runs lengthwise along the curve of the meniscus, following its C-shape. It is often seen in younger, athletic individuals and may respond well to surgical repair, especially when located in the outer third of the meniscus.
A bucket handle tear is a severe form of a vertical tear. In this case, a large portion of the meniscus flips inward into the knee joint, making it difficult to bend or straighten the knee. It often causes locking and typically requires surgery to correct.
A flap tear results in a loose piece of cartilage that creates an uneven edge. This flap may shift with knee motion, causing clicking, catching, or locking. If symptoms are persistent, the loose section is often trimmed during a minor procedure.
A complex tear includes multiple tear patterns—usually both radial and horizontal—and often occurs in worn or degenerated menisci. These are difficult to repair and typically require removal of the damaged sections.
An oblique tear forms at an angle, creating a curved flap that resembles a parrot’s beak. The flap can catch in the joint and lead to sharp pain or instability. Surgical trimming is often used if the tear is unstable.
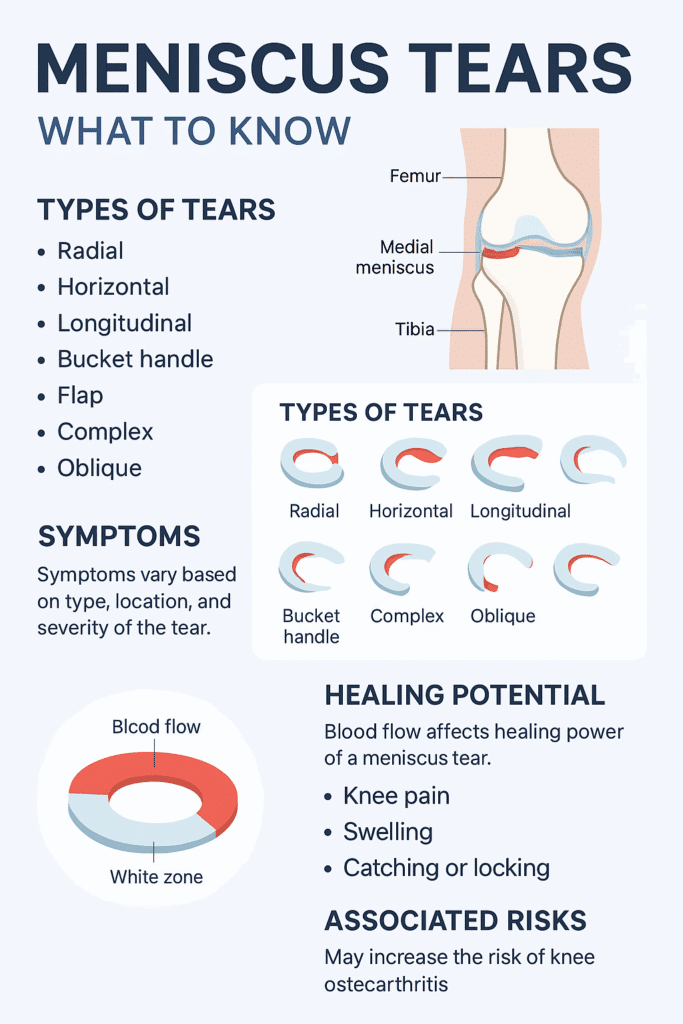
In addition to the shape of the tear, the location is a major factor in symptoms and treatment decisions. These are the meniscus tear locations:
Each location has different mechanical demands, and tears in different areas may feel different or affect how the knee moves.
The meniscus has three zones based on blood supply that affect how well a tear can heal:
How long does it take a meniscus tear to heal? The answer is, it depends. However, if a torn meniscus is left untreated or heals poorly, it can lead to:
Early diagnosis, combined with the right treatment approach, helps protect long-term knee function and mobility.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
Living every day in pain can be debilitating. Imagine waking up each morning already exhausted—not because you didn't sleep, but because your pain kept you tossing and turning all night. Your back aches the moment your feet hit the floor. You grip the bathroom sink for support while brushing your teeth, and getting dressed feels like running a marathon. Driving to work takes every ounce of concentration, not just because of traffic but because your joints throb with every turn. Meetings blur as you shift in your seat, trying to find a less painful position. By the time you get home, you're too sore to cook dinner, too drained to enjoy time with family, and overwhelmed by the idea of another night spent battling discomfort.
This is what daily life can feel like if you're living with chronic pain but it doesn't have to stay this way.
Chronic pain doesn't just hurt your body. It reshapes your life in ways most people never see.
Lower back pain can stem from degenerative disc disease, where the discs between vertebrae lose their cushioning, or herniated discs that press on nerves. Strains, poor posture, or conditions like arthritis and spinal stenosis also contribute.
Dull or Sharp Pain in Your Lower Back
Stiffness or Reduced Flexibility
Radiating Pain into the Buttocks or Legs
Pain That Worsens With Activity or Prolonged Sitting
Muscle Spasms
At POA, we begin with diagnostic imaging and a detailed physical assessment to determine the exact cause of lower back pain. Treatment plans are individualized and may include physical therapy to strengthen core muscles, medication management, and targeted injections. For persistent cases, minimally invasive procedures such as radiofrequency ablation can provide long-term relief.
Options may include:
OA is primarily due to the gradual breakdown of cartilage in joints over time. Risk factors for osteoarthritis include age, obesity, prior joint injuries, and repetitive stress from work or sports.
Joint Pain, Especially After Movement
Swelling and Tenderness
Reduced Range of Motion
Joint Stiffness, Particularly in the Morning
Grating Sensation or Bone Spurs
Managing osteoarthritis means improving function and reducing inflammation without excessive reliance on medications. We may use image-guided joint injections, bracing, and regenerative treatments. Pain doctors also help patients adapt with assistive devices and lifestyle modifications.
Common treatments include:
Often caused by cervical disc herniation or arthritis that compresses spinal nerves. Poor posture, especially with prolonged screen time, is a growing cause in younger adults.
Localized Neck Pain
Radiating Pain Down the Arms
Numbness or Tingling in the Hands or Fingers
Muscle Weakness
Headaches Originating From the Neck
Our team focuses on identifying the source of the nerve compression. We use imaging-guided cervical injections, therapeutic exercises, and posture correction strategies. Nerve blocks or ablation may be used for stubborn pain.
Possible interventions include:
Sciatica is caused by irritation of the sciatic nerve which can often be caused by a herniated disc or bone spur. Spinal stenosis or pelvic trauma may also contribute.
Shooting Pain From the Lower Back Down One Leg
Burning or Tingling Sensations
Weakness in the Leg or Foot
Pain That Worsens When Sitting or Standing for Long Periods
Difficulty Walking
Treatment focuses on reducing nerve inflammation and preventing flare-ups. POA specialists use targeted injections, movement re-education, and sometimes minimally invasive procedures to decompress the nerve.
Treatment strategies may include:
CRPS can develop after surgery, fracture, or sprain. It involves abnormal nerve responses and inflammation that affect the central nervous system's pain regulation.
Severe, Ongoing Pain in One Limb
Swelling and Skin Color Changes
Sensitivity to Touch (Allodynia)
Decreased Mobility or Joint Stiffness
Temperature or Sweating Irregularities
CRPS is complex and requires early, aggressive treatment. Our physicians often use sympathetic nerve blocks, spinal cord stimulation, and desensitization therapy to restore mobility and decrease hypersensitivity.
Interventions may include:
A widespread chronic pain condition that affects muscles and soft tissues, often accompanied by fatigue, memory issues ("fibro fog"), and sleep disturbances.
Symptoms include:
Recurring, often debilitating head pain that can last hours to days. Migraines that are frequently accompanied by nausea, light sensitivity, and aura.
Symptoms can include:
Pain stemming from wear and tear, inflammation, or stiffness of the shoulder joint or tendons. It can severely limit arm function.
Symptoms include:
Pain that persists beyond normal healing after surgery or injury, often involving nerve damage or tissue hypersensitivity.
Symptoms include:
Seeing a pain management doctor at POA isn't just about getting medication or another procedure—it's about reclaiming your life. Our physicians take a whole-person approach to your care. That means listening closely, examining thoroughly, and crafting a treatment plan to meet your needs, lifestyle, and goals.
Whether your pain has lasted months or years, our team is equipped with the tools and experience to make a difference. We blend advanced medical technologies with human compassion. Our goal is to help you move better, sleep longer, work easier, and engage in life again—on your terms.
Pain doesn't need to define who you are or what you can do. With the right care, you can get your life back—and it starts with a conversation at POA.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
You’re bending over to tie your shoe, or maybe you just lifted a laundry basket off the floor—and suddenly, something shifts. A sharp, electric jolt shoots through your lower back and radiates down your leg. Within days, sitting becomes excruciating. You feel tingling in your foot. Or worse—your leg feels weak, like it might buckle underneath you.
It's not just a sore back. You could be dealing with a herniated disc—a spine condition that can disrupt your daily life, mobility, and comfort. But the good news? It’s treatable, and in many cases, you can fully recover without surgery.
Your spine is made up of 33 vertebrae, and between most of them are intervertebral discs—soft, cushion-like pads that absorb shock and allow flexibility in your back.
Each disc has two parts:
A herniated disc, also known as a ruptured disc or colloquially as a “slipped disc”, occurs when the inner core pushes out through a crack or tear in the outer shell. This herniation can press against nearby nerves, triggering pain, numbness, tingling, or weakness—depending on the location and severity of the compression.
Slipped disc vs. herniated disc: While the term "slipped disc" is commonly used, nothing actually “slips” out of place. The disc material bulges or leaks, which is more accurately described as a herniation.
| Herniated Disc | Bulging Disc | |
|---|---|---|
| What it is | The disc's inner gel-like material breaks through a tear in the tough outer layer. The outer wall is torn or ruptured. | The disc extends outward beyond its normal boundary, usually evenly around the disc's circumference. The outer wall remains intact but stretched out. |
| Severity | Typically, more severe than a bulging disc. Especially if it compresses nearby nerves. | Often considered less severe than a herniated disc and can often be asymptomatic. |
| Symptoms | Sharp pain, sciatica, numbness, tingling, or weakness in the limbs. | Mild back pain or none at all. Sometimes asymptomatic. |
| Causes | Trauma, heavy lifting, or progression of a bulging disc. | Degeneration from aging, posture, and repetitive stress. |
| Treatment | May need physical therapy, injections, or even surgery if conservative care fails. | Often responds to conservative care and lifestyle changes. |
Symptoms of a herniated disc depend on the location of the herniation and which nerves are affected. In general, the most common areas are the lumbar (lower back) and cervical (neck) spine.
In many cases, herniated discs heal without surgical intervention. Your body has the ability to reabsorb the protruding disc material and reduce inflammation around the affected nerve.

The recovery timeline depends on the severity of the herniation and the treatment used. It can take time and varies depending on your health, age, and activity level:
| Severity | Differentiator | Recovery Timeframe |
|---|---|---|
| Mild-Moderate | Responds to rest, physical therapy, and medication. | 4-6 weeks |
| Persistent | Involves nerve compression or recurrent flare-ups. | 8-12+ weeks |
| Chronic or Severe | Presents with significant neurological symptoms. | Extensive treatment or surgical intervention |
The most common causes of a herniated disc can include:
If you experience sudden back or neck pain along with radiating symptoms, take the following steps:
Stop any strenuous activity: Avoid lifting, twisting, or bending.
Apply cold packs (for the first 48 hours): Reduces inflammation and pain.
Switch to heat after 2–3 days: Relaxes tight muscles and improves circulation.
Over-the-counter medications: NSAIDs (like ibuprofen) help reduce swelling and pain.
Stay mobile—lightly: Short walks are better than prolonged bed rest, which can weaken muscles and delay healing.
Track your symptoms: Take note of any numbness, tingling, or weakness.
If you suspect you have a herniated disc, don’t wait. If you have any of the following symptoms you should seek care as soon as possible:
For the best outcomes, consult with an orthopaedic specialist. At POA, these may include:
Every person is unique so every treatment approach and plan is tailored for your specific needs.
A typical diagnosis can include a review of your medical history such as prior injuries, sumptom patterns, lifestyle, and your work habits. It also involves a physical exam which may include reflex testing, muscle strength, raings of motion, and nerve response.
Imaging may also be ordered to assist in a comprehensive evaulation.


At POA, we specialize in restoring comfort, strength, and movement—without rushing to surgery.
✅ Board-certified spine specialists with years of experience in both conservative and advanced surgical care.
✅ Personalized treatment plans: Tailored to your body, lifestyle, and goals.
✅ Commitment to conservative care first: We explore every non-surgical option before recommending surgery.
✅ Multidisciplinary approach: Orthopaedic surgeons, physical therapists, and pain specialists collaborate on your care.
✅ Advanced diagnostics: Immediate access to imaging and nerve studies for fast, accurate diagnosis
Whether you’re newly injured or have struggled with back pain for months, POA’s spine experts can help you get your life back on track.
A herniated disc can feel like a life-altering injury, but it doesn’t have to be. With the right care team and a focused treatment plan, recovery is not only possible—it’s probable. Don’t wait in pain! Schedule with one of our Orthopaedic Spine Specialists today and take your first step toward relief and recovery.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
You know the pain well. As you rise from bed every morning, you place your feet on the floor, only to be greeted with a sharp, stabbing sensation in your heel. It's like a jolt that reminds you that the pain isn't gone yet. After walking around for a few minutes, the discomfort may ease. Still, it always comes back when you've been on your feet too long, especially after resting or sleeping. This is a daily struggle for those living with plantar fasciitis – a condition that affects your ability to walk comfortably and can take a toll on your overall quality of life.
Plantar fasciitis occurs when a thick connective tissue running from your heel to your toes along the bottom of your foot (plantar fascia) becomes irritated and inflamed. The plantar fascia supports the foot's arch and is essential for proper foot movement and support while walking. Excessive strain or overstretching can cause tiny tears in the fascia, triggering inflammation and discomfort, particularly in the heel.
While plantar fasciitis is frequently seen in physically active individuals, it can affect anyone. Symptoms tend to worsen in the morning when the tissue tightens during sleep, causing significant discomfort with the day's first steps.
If you’ve ever felt a sharp, stabbing pain in your heel when you step out of bed in the morning, you may be dealing with plantar fasciitis—one of the most common causes of heel pain. This condition affects millions of people each year, but it’s not random. Certain groups are more likely to develop it based on lifestyle, footwear choices, and physical activity.
People who run regularly or participate in high-impact sports are among the most common groups to experience plantar fasciitis symptoms. Repetitive motion, especially without proper stretching or supportive footwear, can cause microtears in the plantar fascia. Increasing mileage too quickly, running on hard surfaces, or using worn-out shoes can all contribute to heel pain in runners.
Working a job that keeps you on your feet for hours at a time can put you more at risk for developing plantar fasciitis. Teachers, nurses, warehouse workers, and retail staff often experience chronic foot and heel pain due to the constant pressure on their feet—especially if they’re standing on hard surfaces like concrete or not wearing cushioned shoes.
Carrying extra weight puts more pressure on your feet and heels, making it harder for your plantar fascia to do its job. This is especially true during long periods of walking or standing. Losing even a modest amount of weight can often reduce pain and prevent further damage.
Your natural foot shape or the way you walk could be behind your chronic heel pain. People with flat feet, high arches, or those who overpronate (roll their feet inward too much) often experience more strain on the plantar fascia, leading to irritation and inflammation. Tight calf muscles or a limited range of motion in your Achilles tendon can also increase your risk.
Unfortunately, age is another common factor. Middle-aged adults are more likely to develop plantar fasciitis due to natural wear and tear. The connective tissue in our bodies loses elasticity as we age, making us more prone to injury from overuse or poor support.
Let’s talk about your footwear! Flip-flops, ballet flats, high heels, and worn-out sneakers all share the same issue, they offer little to no arch support. Wearing these types of shoes regularly can increase your risk of developing plantar fasciitis, especially if you're walking long distances or spending hours on your feet.
Several contributing factors can lead to plantar fasciitis. Understanding these causes of plantar fasciitis can help prevent the condition or reduce the risk of recurrence:
Overuse and repetitive stress
Plantar fasciitis is often caused by repetitive activity that stresses the plantar fascia. High-impact activities like running or jumping can overstrain this tissue, especially if done incorrectly or without proper footwear.
Improper footwear
Shoes that lack adequate arch support, cushioning or are worn-out can exacerbate heel pressure. High heels, flip-flops, or shoes with flat soles may contribute to this strain.
Foot structure abnormalities
People with flat feet, high arches, or abnormal gait patterns may place excessive stress on the plantar fascia. The added strain causes the tissue to become overstretched, leading to inflammation and pain.
Obesity or excess weight
Extra weight puts additional pressure on the feet, making them more susceptible to injury and strain. Over time, this additional weight can cause microtears in the plantar fascia, leading to plantar fasciitis.
Tight calf muscles or Achilles
Having tightness in the calves or Achilles tendon can affect how pressure distributes across your feet. This adds stress to the plantar fascia, increasing the likelihood of inflammation and discomfort.
Aging
As you age, the plantar fascia loses some elasticity and shock-absorbing properties. This makes the tissue more prone to tears and inflammation, leading to plantar fasciitis, especially in people over 40.
Please contact us! We'd love to help.
If you have pain, please contact us and schedule an appointment. We have urgent care facilities all over New Jersey for your convenience.
You can usually manage plantar fasciitis with at-home treatments. Still, sometimes, certain situations warrant a visit to an orthopedic specialist.
Here are several strategies you can use at home to help relieve the pain and inflammation associated with plantar fasciitis:
Giving your foot time to heal is essential. Avoid activities that involve running, jumping, or standing for long periods, as these can further irritate the plantar fascia.
Applying an ice pack to your heel for 15-20 minutes several times throughout the day can help reduce inflammation and pain.
Medications like ibuprofen or naproxen can reduce inflammation and relieve pain. Be sure to follow the recommended dosage and consult a doctor if needed.
Stretching your calf muscles, Achilles tendon, and the plantar fascia can help alleviate your pain and prevent stiffness. Simple exercises like towel stretches or calf stretches can improve your flexibility and reduce the strain on your foot.
Wearing supportive shoes with proper arch support and cushioning can reduce pressure on your plantar fascia. Orthotic insoles may also help distribute pressure more evenly across your foot.
Wearing night splints can help maintain a light stretch of the plantar fascia while you sleep. This helps prevent the fascia from tightening during the night and reduces morning pain.
Preventing plantar fasciitis is possible but it involves making adjustments to your daily habits and lifestyle.

Wear proper footwear – Select footwear that provides the right arch support, cushioning, and stability for your heels. Avoid walking barefoot on hard surfaces and limit prolonged use of high heels to reduce strain on your feet.
Regular Stretching – Regularly stretch your calves, Achilles tendons, and feet to improve flexibility and reduce the risk of strain on the plantar fascia.
Maintain a healthy weight – Keeping your weight within a healthy range will help to reduce the strain on your feet, decreasing your chances of developing plantar fasciitis.
Take breaks to rest – If you stand or walk for long periods, take breaks to rest your feet and alleviate pressure. If you can't take breaks, alternating between sitting and standing can also help prevent overuse.
Strengthen your feet and lower legs – Exercises that strengthen your calf muscles, foot muscles, and ankle stabilizers can help prevent plantar fasciitis by improving foot mechanics and reducing excessive strain.
Towel Stretch – Sitting on the floor with your legs stretched out in front of you, wrap a towel around the ball of your foot. Gently pull your foot toward you, feeling a stretch along the bottom of your foot and the back of your leg.
Calf Stretch – Stand arm's length facing a wall and step back with one leg. Keep your back leg straight and your heel planted on the ground. Place your hands on the wall at the height of your shoulders and lean forward, stretching your calf and Achilles tendon of your back leg.
Foot Roll – To help massage the plantar fascia and relieve built-up tension, you can use a tennis ball or similar ball under the arch of your foot. Once you place it, slowly roll it back and forth.
Toe Stretch – While sitting with your legs extended, reach for your toes and gently pull them toward your body. This stretch helps loosen the plantar fascia and should be held for 15-30 seconds before repeating.
Heel Raises – Stand with the balls of your feet on the edge of a step. Slowly lift yourself onto your toes, then lower your heels past the level of the step to stretch your calves and the bottom of your feet.

Whether you're a runner, a retail worker, or someone who loves their flip-flops a little too much, plantar fasciitis can sneak up on you. Knowing your risk factors is half the battle. With the right footwear, regular stretching, and paying attention to heel pain symptoms, you can take steps (literally!) to protect your feet.
Plantar fasciitis doesn't have to be a permanent issue. You can effectively manage and treat this painful condition with proper care, early intervention, and lifestyle adjustments. If your at-home treatments aren't bringing you relief or if your symptoms are worsening, Princeton Orthopaedic Associates is here to help. Our team of specialists can provide targeted therapies, advanced treatments, and personalized care to help you get back on your feet and live pain-free.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.

You wake up with a stiff neck, thinking you just slept in an odd position. But as the day goes on, the pain doesn't go away. Instead, it radiates down your shoulder and into your arm. Simple tasks like turning your head, reaching for your phone, or even sitting at your desk become uncomfortable. You think, maybe you just slept weird and it will feel better tomorrow, except the pain doesn't improve, it continues for days, even weeks. This is what living with a pinched nerve in the neck can feel like—persistent discomfort that affects your daily life.
A pinched nerve in the neck, also known as cervical radiculopathy, occurs when excessive pressure is applied to a nerve root in the cervical spine (neck area). This pressure can come from surrounding structures such as bones, cartilage, muscles, tendons, or swollen tissues, leading to nerve irritation or compression. This compression disrupts the nerve's normal function and can lead to pain, tingling, weakness, or numbness in your neck.
The symptoms you experience from a pinched nerve in the neck can vary from person to person, but generally speaking, the most common symptoms often involve a discomfort that radiates beyond your neck. You may experience a sharp or burning pain that extends into the shoulder, arm, or even down to the fingers, sometimes worsening with certain movements or prolonged positions. With the pain, there may be an unusual tingling or buzzing sensation, almost like the affected area has "fallen asleep," which can become persistent or intermittent. You may also notice weakness in their grip or find it harder to perform tasks requiring fine motor skills, as the nerve's ability to send signals to the muscles is compromised. In more severe cases, prolonged compression can lead to a feeling of numbness or loss of sensation in certain areas, making it difficult to tell if you're touching something or feeling temperature changes properly.
The causes of a pinched nerve in the neck can vary from person to person, but generally speaking, they stem from excessive pressure or irritation affecting the nerves in your spine in the neck. In many cases, age-related changes in the spine, such as degenerating discs or bone spurs, gradually narrow the space where nerves exit, leading to compression. Injuries, like sudden whiplash from a car accident or repetitive strain from poor posture, can also cause misalignments or inflammation that presses on the nerve. For some people, long hours spent looking down at a phone or sitting at a desk with improper ergonomics contribute to chronic strain, gradually leading to nerve irritation. Inflammatory conditions, like arthritis, or acute issues, such as a herniated disc leaking fluid onto nearby nerves, can also increase pressure, intensifying symptoms over time.
Pain persists for several weeks despite home treatments.
Weakness in your arms or hands affects daily tasks.
Loss of coordination or balance signals nerve damage beyond just discomfort.
Symptoms worsen over time, even with rest and self-care.
Loss of bowel or bladder control can sometimes happen and may indicate a more serious spinal condition requiring immediate attention.

A pinched nerve can cause discomfort ranging from mild tingling to sharp, radiating pain that disrupts daily life. Whether it’s in your neck, back, or another area, this condition occurs when surrounding tissues—such as muscles, tendons, or bones—put excess pressure on a nerve. While severe cases may require medical attention, many pinched nerves can be relieved at home with simple, effective treatments.
Preventing a pinched nerve in the neck starts with maintaining good posture, keeping muscles strong and flexible, and avoiding repetitive strain. Poor posture, prolonged screen time, and sleeping in awkward positions can all contribute to nerve compression, leading to pain, stiffness, and discomfort. By making small adjustments—such as improving ergonomics, incorporating regular stretching, and strengthening the neck and shoulders—you can reduce the risk of nerve irritation and keep your neck healthy and pain-free.
When dealing with a pinched nerve, gentle movement and stretching can help alleviate pressure, improve mobility, and promote healing.
Purpose: Strengthens the deep neck flexors, improves posture, and reduces strain on the cervical spine.
How to Do It:
Tip: Avoid tilting your head up or down—think of sliding your head straight back.
Purpose: Stretches the muscles along the sides of your neck to reduce tension.
How to Do It:
Tip: Keep your shoulders down and relaxed to get the full benefit of the stretch.
Purpose: Increases flexibility and reduces stiffness in the neck.
How to Do It:
Tip: Move slowly and avoid forcing the stretch. If you feel pain, stop immediately.
Purpose: Relieves tension in the shoulders and neck, improving blood flow.
How to Do It:
Tip: Perform this exercise slowly and deliberately, focusing on releasing tension in your upper back and neck.
Purpose: Helps release tightness in the upper shoulders and neck, which can contribute to nerve compression.
How to Do It:
Tip: Keep your opposite shoulder relaxed and down to maximize the stretch.
Perform these exercises gently—never force a stretch.
Consistency is key; do them daily for best results.
If you experience sharp pain or worsening symptoms, stop immediately and consult a healthcare provider.
A pinched nerve in your neck can make daily activities difficult, but you don't have to live with chronic pain. You can find relief and restore normal function with proper care, treatment, and lifestyle adjustments. Our spine specialists here at Princeton Orthopaedics Associates are here to help if your symptoms persist or worsen. Reach out today for expert care and personalized treatment options to get you back to living pain-free.
This blog post is meant to be informative and should not act as a self-diagnosis tool. If you’d like to see one of our doctors, please contact us here.
© 2025 Princeton Orthopaedic Associates. The contents of PrincetonOrthopaedic.com are licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. Copying without permission is strictly forbidden. Privacy Policy | Accessibility